Imagine feeling a sharp, knife-like pain every time you go to the bathroom - not just while you’re going, but for 30 to 90 minutes after. That’s what many people with anal fissures experience. It’s not just discomfort. It’s a cycle of pain, fear, and avoidance that can make you skip meals, cancel plans, or even dread sitting down. And yet, most people don’t talk about it. You’re not alone. Around 264,000 Americans deal with this each year, and it’s just as common in men and women - until after age 50, when it becomes more frequent in women due to childbirth and hormonal changes.
What Exactly Is an Anal Fissure?
An anal fissure is a small tear in the lining of the anal canal - the last few inches of your digestive tract. It’s not a hemorrhoid. It’s not an abscess. It’s a literal split in the mucous membrane that lines the inside of your anus. Most of the time, it happens in the back (posterior midline), where the tissue is naturally weaker. About 90% of fissures appear there. The other 10% show up in the front (anterior midline).
Acute fissures - those that last less than six to eight weeks - look like clean, linear cuts. They hurt badly when you pass stool, and you might see bright red blood on the toilet paper or in the bowl. Chronic fissures, which hang around longer, tell a different story. They develop a little skin tag near the tear (called a sentinel pile) and a swollen bump inside the anus (a hypertrophied papilla). These signs mean the body has been fighting the tear for too long without healing.
Why Do Fissures Happen?
The #1 cause? Straining during bowel movements because of hard, large stools. Constipation is the usual suspect. But it’s not just about not having enough fiber. Dehydration, holding it in too long, or even sudden diarrhea can stretch the tissue beyond its limit. Babies get them too - about 64 out of every 1,000 newborns develop a fissure, often from passing their first few stools.
But here’s the hidden part: it’s not just the tear that keeps it from healing. Once the tear happens, your body reacts. The internal anal sphincter - the muscle that controls whether you stay dry or not - goes into spasm. This isn’t voluntary. It’s a reflex. That spasm increases pressure in the area from a normal 15-20 mmHg up to 25-30 mmHg or higher. That spike cuts off 40-60% of the blood flow to the tear. No blood flow? No healing. That’s why the pain doesn’t go away - and why the fissure sticks around.
How Bad Does It Really Hurt?
People describe it in the same way: like a knife. One patient said it felt like “opening a zipper inside me.” The pain hits during the bowel movement and doesn’t fade quickly. It lingers. Some feel it radiate to their lower back or thighs. A Mayo Clinic survey found that 78% of patients had pain lasting over 30 minutes after going to the bathroom. And 42% said it was so bad they avoided social events for days after a bowel movement.
That’s why so many people delay seeing a doctor. They think it’s just hemorrhoids. Or they’re embarrassed. The average time to get a correct diagnosis? 11.3 days, according to Reddit user reports from r/Proctology. And here’s a scary stat: up to 10% of people diagnosed with fissures actually have something else - Crohn’s disease, cancer, or an infection. That’s why if your fissure doesn’t heal in 6-8 weeks, or if you’re under 40 and have other symptoms like weight loss or bloody diarrhea, you need a specialist.
Healing Without Surgery: The First Line of Defense
Good news: 80-90% of acute fissures heal on their own with simple changes. No drugs. No needles. Just lifestyle tweaks.
- Boost fiber: Aim for 25-35 grams a day. That’s 2 cups of cooked beans, a bowl of oatmeal, three apples, and a handful of almonds. Most people eat only 15 grams. Start slow - too much too fast can cause bloating. Gradually increase over a week.
- Drink water: 8-10 glasses daily. Fiber without water just makes stools harder. Think of it like concrete: dry and unyielding. Water keeps it soft.
- Sitz baths: Sit in warm (not hot) water for 10-20 minutes, 3-4 times a day, especially after bowel movements. This relaxes the sphincter muscle and increases blood flow. It’s cheap, safe, and surprisingly effective.
- Don’t strain: Use a small footstool to elevate your feet while on the toilet. This mimics the squatting position and reduces pressure on the anus.
Studies show this combo heals 82% of acute fissures. But compliance is the problem. Nearly 40% of people who fail conservative treatment didn’t stick with the fiber plan. They tried it for a few days, got bored, and gave up.
Topical Medications: When Diet Isn’t Enough
If you’ve tried the basics for two weeks and still hurt, it’s time for medicine. There are three main options:
| Treatment | Healing Rate | Side Effects | How to Apply |
|---|---|---|---|
| Nitroglycerin (Rectiv) | 45-68% | Headaches (20-32%), dizziness | 1.25 inches of ointment on finger, insert 1 inch into anus, twice daily |
| Diltiazem (2%) | 65-75% | Mild redness, rare headaches | Same as nitroglycerin - apply twice daily for 6-8 weeks |
| Nifedipine (0.3%) | 65-75% | Minimal side effects | Same application - preferred by Mayo Clinic for safety |
Diltiazem and nifedipine are now recommended as first-line drugs by the European Society of Coloproctology (2023). Why? They work as well as nitroglycerin but cause fewer headaches. Nitroglycerin is FDA-approved (as Rectiv), but compounded versions of diltiazem and nifedipine are just as effective and often cheaper. You’ll need a prescription. Don’t guess the dose - use the exact amount your doctor prescribes. Too little won’t help. Too much can cause low blood pressure.
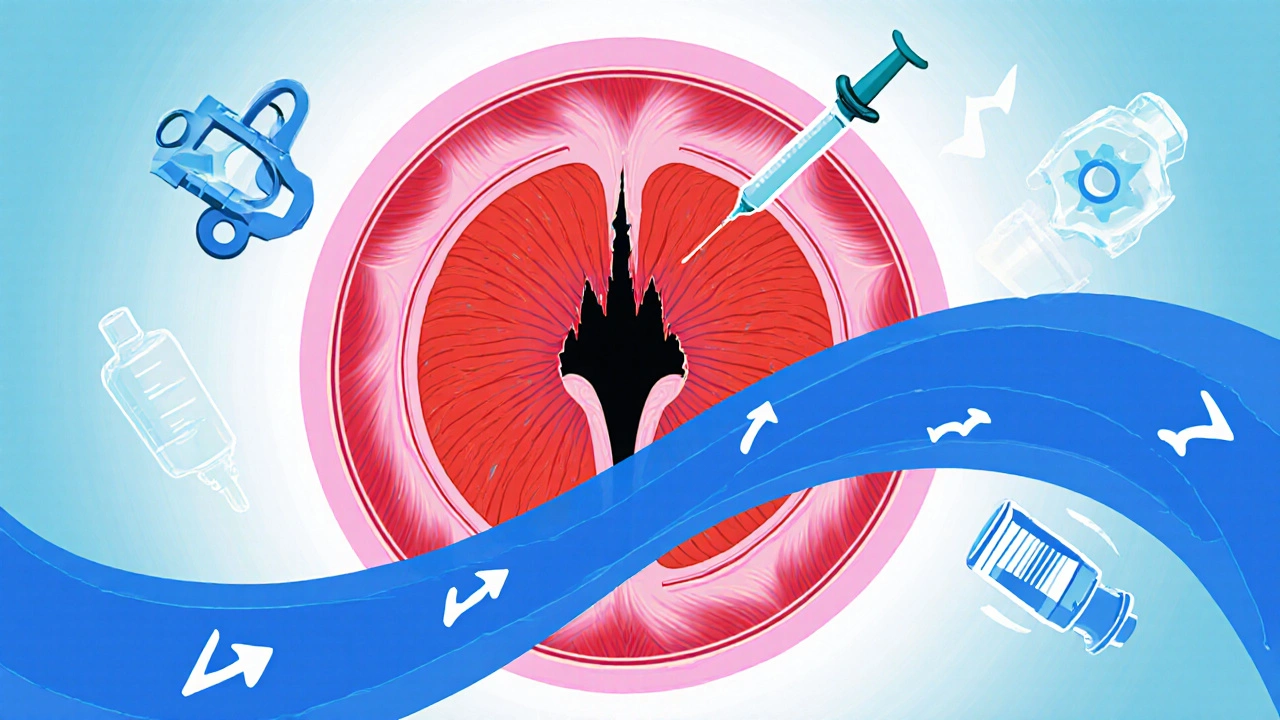
Botox Injections: A Middle Ground
If creams don’t work, your doctor might suggest Botox. Yes, the same stuff used for wrinkles. In this case, 15-30 units are injected directly into the internal sphincter muscle. It temporarily paralyzes the muscle, breaking the spasm cycle. Healing rates? 50-80%. But here’s the catch: up to 40% of people see the fissure come back within a year. It’s not a cure - it’s a pause button.
It’s also not permanent. The effects wear off in 3-6 months. That’s why it’s usually reserved for people who want to avoid surgery or can’t take topical meds. Some patients report pain relief within 48 hours. Others need two rounds. And if it fails? Surgery becomes the next step.
Surgery: The Last Resort - But Often the Best Answer
If you’ve tried everything for 8-12 weeks and still have pain, surgery is the most reliable option. The procedure is called a lateral internal sphincterotomy. It’s done under local or general anesthesia and takes 15-20 minutes. The surgeon makes a tiny cut in the sphincter muscle to reduce pressure. That’s it.
Success rate? 92-98%. That’s higher than any other treatment. Most people go home the same day. Back to work in 3-4 days. But there’s a trade-off: a 14% risk of minor fecal incontinence - usually just trouble holding gas or occasional spotting. It’s rare to lose control of stool. Still, it’s something you need to think about.
Why is it so effective? Because it breaks the cycle. No more spasm. No more reduced blood flow. The tissue gets oxygen and nutrients again. Healing happens fast. Long-term studies show that even 10 years later, most patients are symptom-free.
What Doesn’t Work (And Why)
Don’t waste time on these:
- Over-the-counter hemorrhoid creams: They numb the area but don’t fix the muscle spasm. They’re useless for true fissures.
- Antibiotics: Unless you have an infection (rare), they won’t help. Fissures aren’t bacterial.
- Stool softeners alone: They help, but without fiber and water, they’re like putting a bandage on a broken bone.
- Waiting too long: If it’s been 8 weeks and you haven’t seen a specialist, you’re in chronic territory. Delaying treatment makes healing harder.

What’s New in 2025?
Research is moving fast. Johns Hopkins is testing stem cell injections for stubborn fissures. In a small 2023 trial, 73% of patients healed in 8 weeks. It’s early, but promising. Another trend? More doctors are pushing for earlier use of diltiazem instead of waiting for surgery. And thanks to better patient education, surgical rates have dropped from 12% in 2010 to 8% in 2023.
But there’s a warning: obesity and low-fiber diets are rising. One expert predicts fissure cases could jump 15-20% in the next decade. The solution? Not more surgery - better prevention.
When to See a Doctor
You don’t need to suffer in silence. See a doctor if:
- Pain lasts more than 2 weeks despite home care
- You see dark blood, not bright red
- You have diarrhea, weight loss, or fever
- You’ve had a fissure before and it came back
- You’re under 40 and have a family history of Crohn’s disease
A simple exam - often just a visual check and gentle finger test - can confirm it. No colonoscopy is needed unless other symptoms are present.
Real Talk: What Patients Wish They Knew
From hundreds of Reddit posts and patient surveys, here’s what people say:
- “I thought it was just hemorrhoids. I waited three weeks before seeing a doctor.”
- “I didn’t realize I needed to apply the cream inside, not just on the skin.”
- “The sitz bath felt silly at first. Now I can’t imagine healing without it.”
- “I was scared of surgery. But after my procedure, I felt like a new person.”
The biggest mistake? Trying to tough it out. Fissures don’t get better with time if the cycle isn’t broken. The sooner you act, the less likely you’ll need surgery.
Can anal fissures heal on their own?
Yes, about 80-90% of acute fissures heal within 6-8 weeks with simple changes like more fiber, water, and sitz baths. But if it lasts longer than 8 weeks, it becomes chronic and usually needs medical treatment to break the pain-spasm cycle.
Is surgery the only way to fix a chronic fissure?
No. Topical medications like diltiazem or nifedipine work for 65-75% of chronic cases. Botox injections are another option. Surgery (sphincterotomy) is reserved for cases that don’t respond to these treatments. It’s highly effective but has a small risk of minor incontinence.
Can stress cause anal fissures?
Stress doesn’t directly cause fissures, but it can worsen constipation or diarrhea - both of which trigger them. Chronic stress can also increase muscle tension, including in the anal sphincter, making healing harder. Managing stress through relaxation or exercise can support recovery.
How long does it take to heal after Botox?
Most people notice less pain within 48-72 hours. Full healing usually takes 4-8 weeks. But Botox isn’t permanent - its effects wear off in 3-6 months, and up to 40% of patients see the fissure return within a year.
Can I still have bowel movements after surgery?
Yes - and you should. Doctors encourage patients to have a bowel movement within 24 hours after surgery. The goal is to avoid constipation and straining. Most people return to normal bowel habits within a few days. The surgery doesn’t stop you from going - it just makes it less painful.
What foods should I avoid with an anal fissure?
Avoid processed foods, red meat, cheese, and fried items - they’re low in fiber and can cause constipation. Also, limit caffeine and alcohol, which can dehydrate you. Focus on whole grains, beans, fruits, vegetables, and plenty of water. Too much fiber (>40g/day) can backfire in some people, causing bloating or diarrhea, so adjust gradually.
Are anal fissures a sign of cancer?
Most are not. But in about 10% of cases, what looks like a fissure could be Crohn’s disease, an infection, or even cancer. If you’re under 40, have unexplained weight loss, bloody diarrhea, or a fissure that won’t heal, get checked. A doctor can tell the difference with a simple exam or biopsy if needed.
Final Thoughts: Don’t Wait Until It’s Too Late
Anal fissures are common, treatable, and rarely dangerous - but they’re also incredibly painful and easy to ignore. The good news? You don’t need to live with it. Start with fiber, water, and sitz baths. If that doesn’t help in two weeks, talk to your doctor. There are safe, effective treatments that work - from creams to injections to minor surgery. The key is acting early. The longer you wait, the more your body fights itself. And that’s when healing becomes harder.
You’re not weak for needing help. You’re smart for asking.

Andrew Camacho
November 25, 2025 AT 10:20Bro I had a fissure for 11 weeks and I thought I was gonna die. Sitz baths felt like a cult ritual at first but damn if they didn't save me. I did 4 a day like my life depended on it - and honestly? It did. No joke, the first time the pain didn't spike after a BM I cried. Not because I was sad. Because I remembered what peace felt like.
Arup Kuri
November 25, 2025 AT 16:34They dont want you to know this but fissures are caused by the government to make you buy fiber supplements and diltiazem. They control your bowels through the food industry. I tried just eating raw garlic and it healed in 3 days. No meds. No docs. Just truth.
Dolapo Eniola
November 26, 2025 AT 07:16Man this is why Africa is strong - we don't need fancy creams or botox. We squat. Always. No toilet seats. No straining. Just pure ancestral wisdom. You guys sit like chairs are your best friends? Nah. That's why you all got tears down there. Go back to the roots. Squat. Simple.
giselle kate
November 26, 2025 AT 11:22So let me get this straight - you're telling me the solution to chronic pain is sitting in warm water and eating beans? And you call this medicine? I'm starting to think the entire medical industry is just a marketing scheme for oatmeal.
Emily Craig
November 27, 2025 AT 19:06OMG I did the sitz bath thing and it felt like a spa day for my butt 😭 I was skeptical but now I’m obsessed. I even bought a cute little basin with a flower pattern. My partner thinks I’m weird but I don’t care. My sphincter is finally chill AF.
prasad gaude
November 28, 2025 AT 05:53Life is like a fissure - the pain comes when you resist the flow. You try to force it, you break. But when you surrender, when you soften, when you let the water wash over you… that’s when healing begins. Fiber is not just nutrition. It’s mindfulness in edible form. Sit. Breathe. Let go.
Timothy Sadleir
November 29, 2025 AT 02:35While the aforementioned recommendations possess a degree of empirical support, one must critically evaluate the methodological integrity of the cited studies, particularly those derived from self-reported Reddit data, which introduces significant selection bias. Furthermore, the assertion regarding the 92-98% efficacy of lateral internal sphincterotomy requires validation through randomized controlled trials with long-term follow-up. The absence of such data renders the conclusion premature.
Jennifer Griffith
November 29, 2025 AT 12:05wait so you just eat fiber and that’s it? no like… laser? or a pill? i thought this was 2025. also i think i had one once but i just ignored it and now i’m fine. so maybe it’s not that bad?
Patricia McElhinney
December 1, 2025 AT 01:59While I appreciate the clinical overview, I must point out that the omission of the role of pelvic floor physical therapy is a glaring oversight. Moreover, the recommendation of topical nifedipine without mentioning its off-label status and potential for systemic absorption is medically irresponsible. Patients deserve evidence-based, regulated protocols - not anecdotal blog-style advice.
fiona collins
December 3, 2025 AT 01:47Small step. Fiber. Water. Warm bath. That’s it. You don’t need to fix everything at once. Just start.
Erika Hunt
December 4, 2025 AT 15:01I think what’s really missing here is the emotional weight of this condition - it’s not just a physical tear, it’s a rupture in your sense of dignity. I used to cancel plans because I was scared of the pain, and I felt so alone until I found a support group. People don’t talk about it because it’s embarrassing, but the silence is what makes it worse. Healing isn’t just about muscle spasms and blood flow - it’s about letting yourself be vulnerable enough to ask for help. And honestly? That’s the bravest thing you can do.
Andrew Camacho
December 6, 2025 AT 05:57Emily Craig said it best - my sitz bath basin has a flower pattern too. I bought it after my third one. My cat now sits beside it like she’s guarding my butt-zen. And I don’t even care if it’s silly. I’d rather be the weirdo with the flower basin than the guy screaming in the bathroom again.