Antibiotic-Warfarin Interaction Checker
Check Your Antibiotic Safety
Select an antibiotic to see its interaction risk with warfarin and get specific monitoring guidance.
Safety Assessment
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance - sometimes with life-threatening results. It's not just a theoretical risk. Every year, thousands of people on warfarin end up in the emergency room because their INR spiked after starting an antibiotic. And in many cases, it was completely preventable.
Why Antibiotics and Warfarin Don't Mix
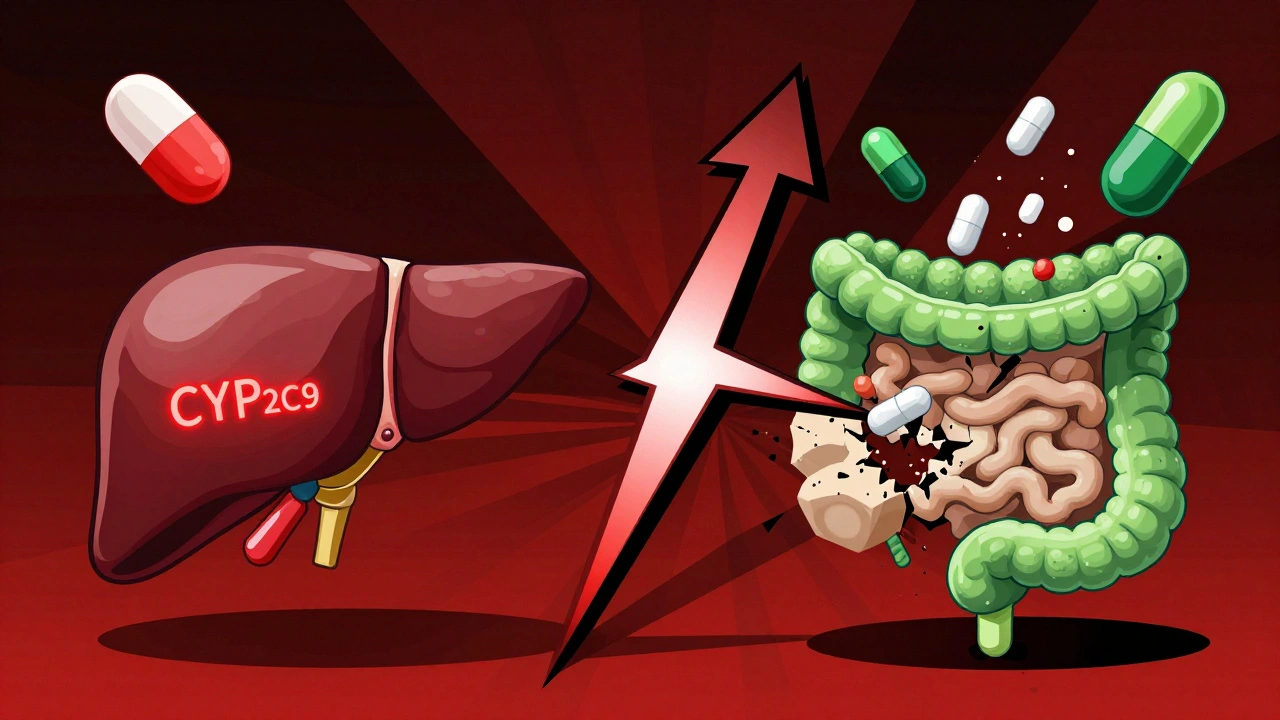
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a tightrope walk: too little, and you risk clots; too much, and you bleed. The therapeutic range for most people is an INR between 2.0 and 3.0. Once it hits 4.0 or higher, your risk of serious bleeding - like brain hemorrhage or internal bleeding - jumps by 4 to 8 times. Antibiotics mess with warfarin in two main ways. First, they kill off the good bacteria in your gut that make vitamin K. Second, they interfere with the liver enzymes (CYP2C9, mainly) that break down warfarin. Either way, warfarin builds up in your system, and your INR climbs.Which Antibiotics Are the Biggest Risks?
Not all antibiotics are created equal when it comes to warfarin. Some are quiet. Others are loud and dangerous. Ciprofloxacin and other fluoroquinolones are among the worst offenders. Studies show they can push INR from 2.5 to 4.1 in under a week. One meta-analysis found people on ciprofloxacin were more than twice as likely to bleed compared to those not taking it. Bactrim (sulfamethoxazole/trimethoprim) is just as bad - it spikes INR by an average of 1.8 units within five days. Erythromycin, a macrolide, increases bleeding risk by 2.3 times. These aren’t rare events. GoodRx data shows these three antibiotics account for nearly 70% of all warfarin-related ER visits. Then there are the sneaky ones. Amoxicillin/clavulanate and some cephalosporins like cefotetan don’t inhibit liver enzymes at all. But they wipe out gut bacteria. That means vitamin K production drops. The INR doesn’t spike right away - it creeps up after 5 to 7 days. That’s why people think they’re safe: they’ve been on the antibiotic for a week and feel fine. Then, suddenly, they bruise easily or notice blood in their stool. On the flip side, azithromycin and ceftriaxone are much safer. Azithromycin barely touches CYP enzymes, and ceftriaxone doesn’t disrupt gut flora much. Rifampin is the opposite - it speeds up warfarin breakdown, causing INR to crash. That’s dangerous too, because now you’re at risk for clots.When Does the Danger Peak?
Timing matters. If an antibiotic blocks warfarin metabolism (like ciprofloxacin), your INR can rise within 2 to 3 days. But if it’s killing gut bacteria (like amoxicillin), the spike comes later - usually between days 5 and 14. And here’s the kicker: the risk doesn’t vanish when you stop the antibiotic. Gut bacteria take 7 to 10 days to recover. So even after you finish your pills, your INR can still climb. A 2012 study of over 31,000 Medicare patients found the highest bleeding risk occurred between days 8 and 14 of antibiotic use. That’s why checking your INR only on day 3 isn’t enough. You need to keep checking - even after the antibiotic is gone.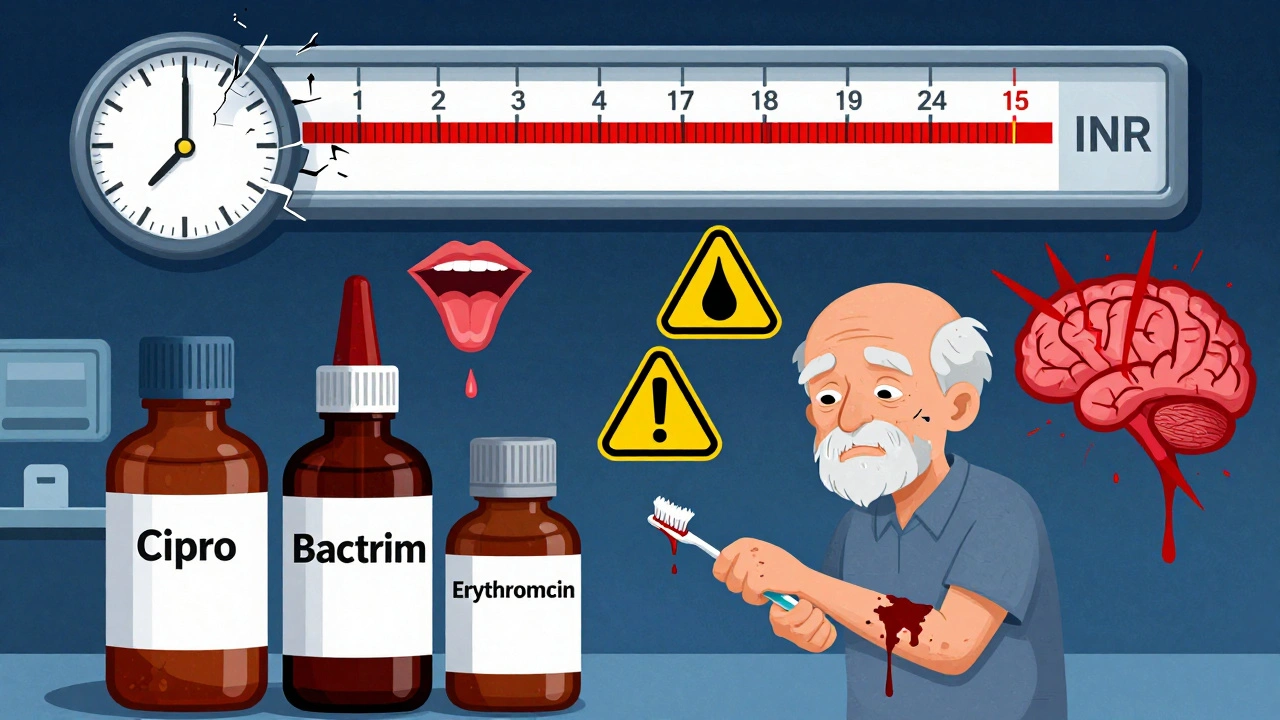
What Should You Do?
If you’re on warfarin and your doctor prescribes an antibiotic, don’t assume it’s safe. Ask these questions:- Is this antibiotic known to interact with warfarin?
- Can we use a safer alternative?
- When should I get my INR checked?
- For high-risk antibiotics (ciprofloxacin, Bactrim, erythromycin): Reduce your warfarin dose by 20-30% on day one. Check your INR every 2-3 days. Keep checking for at least 7 days after stopping the antibiotic.
- For gut-flora disruptors (amoxicillin/clavulanate, cefotetan): No need to change your dose upfront. But check your INR weekly, starting at day 5. Only adjust if your INR goes above your target range.
- For rifampin: You’ll likely need a 50-100% warfarin dose increase. Daily INR checks for the first week are critical.
What to Watch For
You don’t need to wait for your next blood test to know something’s wrong. Learn the warning signs:- Unexplained bruising - especially large, dark patches
- Bleeding gums when brushing your teeth
- Nosebleeds that won’t stop
- Red or dark urine
- Black, tarry, or bloody stools
- Severe headaches, dizziness, or confusion (possible brain bleed)
Who’s Most at Risk?
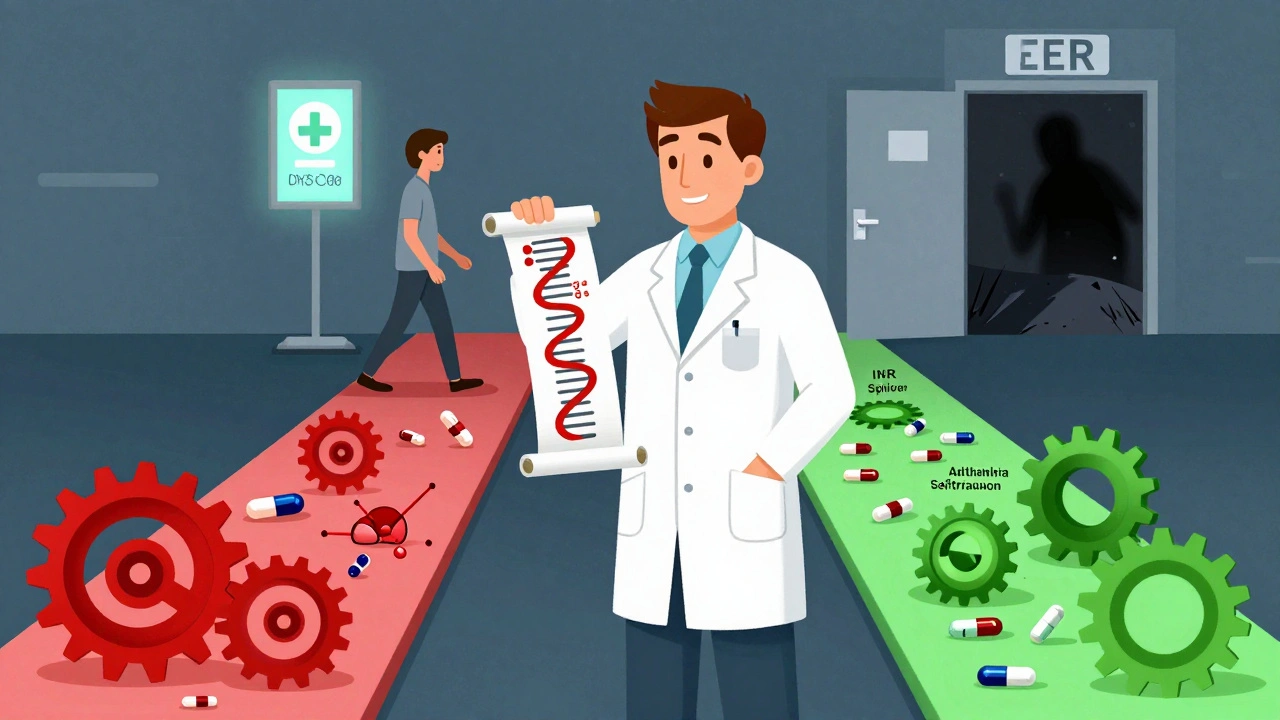
Older adults are hit hardest. About 15-30% of all warfarin-related hospitalizations involve antibiotics. Medicare data shows patients over 65 are 2.3 times more likely to bleed during antibiotic therapy than younger patients. Why? Their livers process drugs slower. Their gut flora is already less stable. And they’re more likely to be on multiple medications. People with CYP2C9 gene variants (like *2 or *3) are also at higher risk. These genetic differences make warfarin harder to break down. When antibiotics block the already-slow pathway, INR spikes even faster. Genetic testing isn’t routine yet - but if you’ve had multiple unexplained INR spikes, it’s worth asking your doctor about it.What’s Changing in 2025?
New guidelines are pushing for smarter monitoring. Pharmacist-led warfarin clinics reduce bleeding complications by 37% compared to doctor-only care. Electronic alerts in EHR systems help - but only if they’re paired with clinical decision support. Just popping up a warning without clear instructions? That doesn’t help. Research is moving toward personalized dosing. The 2023 WARF-GEN trial showed that using genetic data to adjust warfarin before starting an antibiotic cut INR instability by 41%. That’s huge. In the next few years, we may see routine genetic screening for people starting long-term warfarin therapy.Bottom Line: Stay in Control
Antibiotics are essential. Warfarin saves lives. But together, they’re a ticking time bomb if you don’t know how to handle them. Don’t wait for a problem to happen. Before you take any new antibiotic:- Check with your anticoagulation provider
- Know if it’s high-risk or low-risk
- Plan your INR checks - don’t just rely on your next scheduled one
- Know the bleeding signs - and act fast
Clare Fox
December 7, 2025 AT 00:03Kay Jolie
December 7, 2025 AT 10:03Inna Borovik
December 8, 2025 AT 18:22Jackie Petersen
December 10, 2025 AT 18:08Annie Gardiner
December 11, 2025 AT 22:33Rashmi Gupta
December 12, 2025 AT 00:44Andrew Frazier
December 13, 2025 AT 00:17Kumar Shubhranshu
December 14, 2025 AT 00:42Mayur Panchamia
December 15, 2025 AT 04:38Geraldine Trainer-Cooper
December 16, 2025 AT 14:55Nava Jothy
December 17, 2025 AT 06:27Kenny Pakade
December 18, 2025 AT 06:44brenda olvera
December 19, 2025 AT 19:23