Most people don’t realize how much they rely on hearing until it starts slipping away. Maybe you’ve been asking people to repeat themselves more often. Or you turn the TV up too loud. Maybe your kids say you’re not listening, but you swear you heard them. These aren’t just annoyances-they could be early signs of hearing loss. The only way to know for sure is through audiometry testing.
What Is Audiometry Testing?
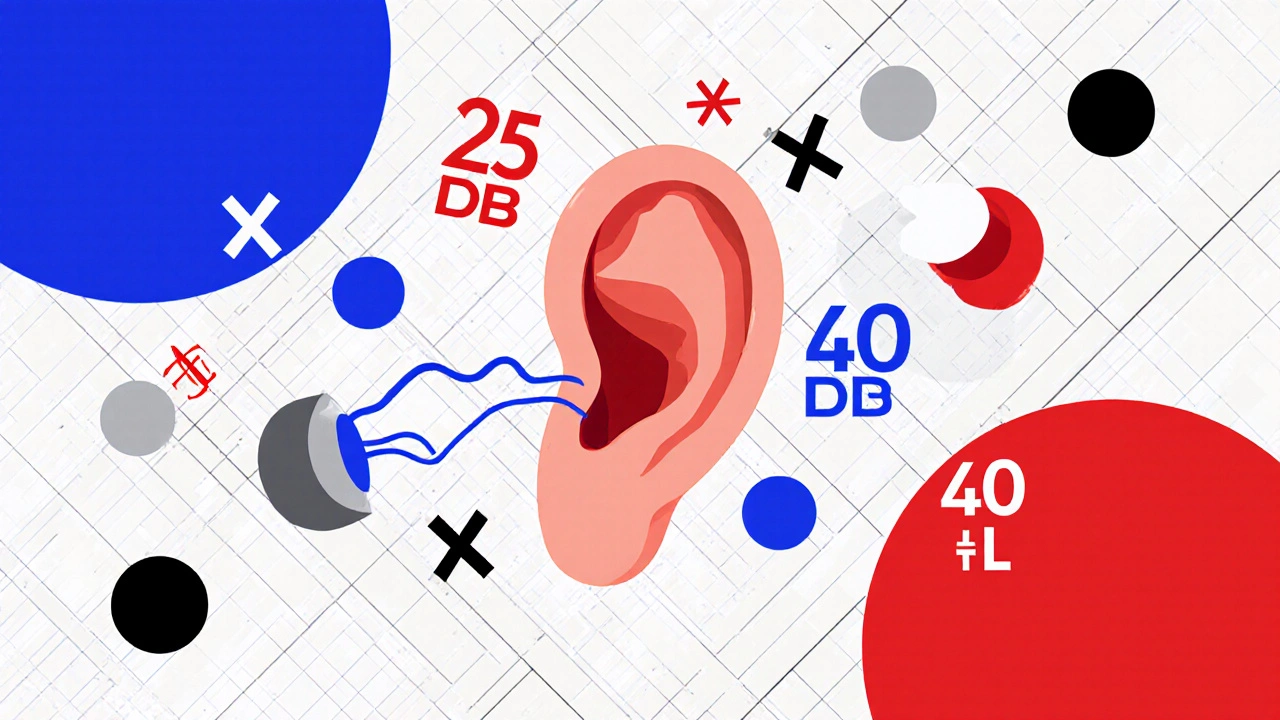
Audiometry testing is the standard way doctors measure how well you hear. It’s not a guess. It’s not a quick beep test at a pharmacy. It’s a detailed, controlled process that maps out exactly what sounds you can and can’t hear across different pitches-like low rumbles and high whistles.The test measures your hearing threshold: the quietest sound you can detect at least half the time. These thresholds are recorded in decibels hearing level (dB HL). Normal hearing is 25 dB HL or better across all tested frequencies. If your threshold is 40 dB at 2000 Hz, that means you need sounds to be 40 decibels louder than what most people with healthy hearing can detect. That’s the difference between hearing a whisper and needing a normal conversation volume to catch every word.
The most common type is pure-tone audiometry. You sit in a quiet room, wear headphones, and press a button every time you hear a tone. The tones start loud and get softer, then back up again. This back-and-forth method, called the modified Hughson-Westlake technique, is used because it’s the most accurate way to find your true threshold. It’s not magic-it’s science. And it’s been the gold standard since the 1940s.
How Air and Bone Conduction Testing Work
There are two main ways sound reaches your inner ear: through the air and through your bones.Air conduction testing uses headphones. Sound travels through your ear canal, vibrates your eardrum, moves tiny bones in your middle ear, and finally reaches the cochlea-the snail-shaped organ in your inner ear that turns sound into signals your brain understands.
Bone conduction testing skips the outer and middle ear entirely. A small device is placed behind your ear, on the mastoid bone. It sends vibrations directly through your skull to the cochlea. If your bone conduction thresholds are normal but your air conduction thresholds are worse, that means something’s blocking sound in your outer or middle ear-like earwax, fluid from an infection, or a perforated eardrum. This is called conductive hearing loss.
If both air and bone conduction are equally poor, the problem is in your inner ear or auditory nerve. That’s sensorineural hearing loss, the most common type, often caused by aging, noise exposure, or genetics.
The difference between air and bone thresholds is called the air-bone gap. If it’s 15 dB or more at any frequency, it points to a conductive issue. Audiologists use this gap to decide whether you need a hearing aid, surgery, or just monitoring.
Speech Testing: More Than Just Tones
Hearing tones is one thing. Understanding speech is another. That’s why every full audiometry test includes speech testing.Speech Reception Threshold (SRT) testing asks you to repeat simple two-syllable words like "baseball" or "hotdog" at decreasing volumes. The goal is to find the lowest level where you get half of them right. Your SRT should match your average pure-tone threshold at 500, 1000, and 2000 Hz-within 10 dB. If it doesn’t, something’s off. Maybe you’re not paying attention. Or maybe your brain is struggling to process sound, even if your ears are picking it up.
Then comes speech discrimination testing. You hear words at a volume you can clearly hear, and you repeat them back. A healthy listener gets 90% or more correct. If you’re only getting 60%, that’s a red flag. You might have sensorineural hearing loss, or even a problem with the auditory nerve. Some people with normal audiograms still struggle in noisy rooms. Their speech scores explain why.
Tympanometry: Checking the Middle Ear
Audiometry isn’t just about what you hear. It’s also about how well your ear works mechanically.Tympanometry checks your eardrum’s flexibility. A small probe seals your ear canal and changes the air pressure while playing a tone. It measures how much your eardrum moves. The result is a graph called a tympanogram.
A normal result looks like a hill-your eardrum moves easily. A flat line (Type B) means fluid is trapped behind your eardrum, common in ear infections. A very high peak (Type C) suggests negative pressure, often from Eustachian tube dysfunction. This test takes less than five seconds per ear and helps audiologists rule out middle ear problems before recommending hearing aids.
What About Babies and Non-Responsive Patients?
Adults can press a button when they hear a tone. Babies can’t. That’s where objective tests come in.Auditory Brainstem Response (ABR) testing uses electrodes on the scalp to measure how your brainstem reacts to clicking sounds. It doesn’t need you to respond. It’s used for newborns, young children, and people who can’t reliably answer questions. The CDC recommends all newborns get screened before leaving the hospital. If they fail, a full diagnostic ABR must be done by three months old. Early detection means early intervention-and better outcomes.
For toddlers, visual reinforcement audiometry (VRA) turns the test into a game. When the child turns toward a sound, a toy lights up or dances. Parents often say their kids think it’s fun. It’s not just clever-it’s effective. Studies show VRA gives accurate results even for 12-month-olds.
Understanding Your Audiogram
After the test, you’ll get a chart called an audiogram. It looks like a graph with frequency (pitch) on the bottom and loudness (decibels) on the side.Each ear is marked differently: circles for right ear air conduction, X’s for left ear air conduction. Bone conduction is shown with brackets for the right ear and less-than signs for the left. If you see a gap between the circles and the brackets, that’s your air-bone gap.
Here’s what the lines mean:
- 0 to 25 dB HL: Normal hearing
- 26 to 40 dB HL: Mild hearing loss-miss soft speech, struggle in noise
- 41 to 55 dB HL: Moderate hearing loss-need to ask people to repeat, TV too loud
- 56 to 70 dB HL: Moderately severe-can’t hear most conversations without hearing aids
- 71 to 90 dB HL: Severe-only hear loud sounds, hearing aids essential
- 91+ dB HL: Profound-may rely on lip-reading or sign language
Some people have a "notch" at 4000 Hz-a dip in hearing at a high pitch. That’s classic noise-induced hearing loss. It often starts with jobs like construction, music, or military service. It’s preventable. But once it’s there, it’s permanent.
Why Accuracy Matters
Audiometry isn’t just about getting a number. It’s about getting the right number. If your audiometer isn’t calibrated correctly, or if masking isn’t used when needed, your results could be wrong.For example, if your right ear hears much better than your left, the sound from the right headphone might leak into your left ear. That’s called crossover. To stop that, audiologists use noise to mask the good ear while testing the bad one. About 12% of tests fail because masking wasn’t done right, according to Mayo Clinic data.
ANSI standards require audiometers to be checked yearly to stay within ±3 dB of accuracy. That’s the difference between recommending a hearing aid and saying you’re fine. Don’t settle for a quick screening if you’re having real trouble. Get a full diagnostic test.
Who Needs Audiometry Testing?
You don’t have to wait until you’re struggling. Here’s who should get tested:- Anyone over 50-hearing loss becomes more common with age
- People exposed to loud noise regularly-construction, factories, concerts, firearms
- Those with a family history of hearing loss
- People taking ototoxic medications-some antibiotics, chemotherapy drugs, and high-dose aspirin
- Anyone with ear pain, fullness, ringing (tinnitus), or dizziness
- Children who don’t respond to their name or seem to ignore speech
The National Institute on Deafness and Other Communication Disorders estimates 48 million Americans have hearing loss. But only about 1 in 3 people over 70 who could benefit from hearing aids actually use them. Why? Often because they don’t know how bad it is. Audiometry gives you the facts.
What to Expect During the Test
The whole process takes 30 to 45 minutes. You’ll be asked to sit quietly, wear headphones, and respond to sounds. No pain. No needles. Just a quiet room and a button to press.Some people find bone conduction uncomfortable, especially if they wear glasses. The oscillator can press against the frame. Tell your audiologist if it’s bothering you-they can adjust the placement.
Afterward, they’ll walk you through your audiogram. They’ll explain what the numbers mean for your daily life. Do you need hearing aids? Can you still drive safely? Will you miss your grandchild’s first words? These aren’t just technical questions-they’re life questions.
One patient in Toronto told me: "The audiologist showed me my audiogram and pointed to the 45 dB dip at 2000 Hz. That’s where consonants like S, T, and K live. Suddenly, I understood why I kept missing words like ‘cat’ or ‘bus.’ It wasn’t that I wasn’t listening. I just couldn’t hear them."
Where to Get Tested
You can get a basic screening at a pharmacy or retail hearing center. But for a full diagnostic test, go to an audiologist. They have the training, equipment, and time to do it right.Look for clinics affiliated with hospitals or universities. They follow ASHA and ANSI standards. Avoid places that push hearing aids before testing. A good audiologist will explain your options, including whether you even need a device.
Tele-audiology is growing. Some companies offer remote testing with validated equipment like the KUDUwave booth. But it’s not perfect. It can’t reliably detect thresholds below 25 dB HL, and it doesn’t replace in-person tympanometry or speech testing.
What Happens After the Test?
If your hearing is normal, great. Keep protecting it. Wear earplugs at concerts. Turn down the volume. Get checked again in three years.If you have mild to moderate hearing loss, hearing aids are the most common solution. Modern devices are tiny, smart, and can connect to your phone. They don’t make you hear perfectly-but they make conversations possible again.
If you have a conductive issue, you might be referred to an ENT surgeon. Fluid, wax, or a stiff stapes bone can often be fixed. Surgery isn’t always needed, but it’s an option.
For severe loss, cochlear implants might be considered. But that’s only after a full evaluation.
The key is action. Hearing loss doesn’t get better on its own. The longer you wait, the harder it is for your brain to relearn how to process sound. Studies show people who get hearing aids within a year of diagnosis do better than those who wait five years.
Is audiometry testing painful?
No, audiometry testing is completely painless. You’ll wear headphones or have a small device placed behind your ear, but there’s no pressure, needles, or discomfort. Some people find bone conduction vibrations slightly odd, especially if they wear glasses, but it’s not painful.
How long does an audiometry test take?
A full diagnostic audiometry test usually takes 30 to 45 minutes. This includes pure-tone testing, speech testing, tympanometry, and a results review. Screening tests can be done in under 10 minutes, but they don’t give you the full picture.
What does 25 dB HL mean in everyday terms?
25 dB HL is the threshold for normal hearing. It’s about the volume of a quiet whisper from across the room. If you can hear sounds at this level, your hearing is considered healthy. Anything above 25 dB means you need sounds to be louder to detect them.
Can I test my hearing at home with an app?
Home apps can give you a rough idea, but they’re not reliable for diagnosis. Phone speakers aren’t calibrated, background noise interferes, and earphones vary widely. Only clinical audiometry with calibrated equipment and professional oversight can give accurate, actionable results.
Do I need a referral to get an audiometry test?
In most cases, no. Audiologists are primary care providers for hearing. You can book an appointment directly. However, if you have insurance, your plan may require a referral from your doctor for coverage.
How often should I get my hearing tested?
If you’re over 50 or exposed to loud noise regularly, get tested every year. If you’re under 50 with no risk factors, every three years is fine. If you notice changes-like difficulty understanding speech in noise or ringing in your ears-get tested right away.
Can hearing loss be reversed?
Sensorineural hearing loss-caused by aging or noise damage-is permanent. But it can be managed effectively with hearing aids or cochlear implants. Conductive hearing loss, caused by blockages or infections, can often be reversed with medical or surgical treatment.
Next Steps: Protect Your Hearing
If you’ve never had your hearing tested, don’t wait for it to get worse. Hearing loss creeps in slowly. You adapt. You think you’re fine. But your brain is working harder than it should.Start by finding a licensed audiologist near you. Ask if they follow ASHA guidelines. Ask if they use calibrated equipment. Ask to see your audiogram. A good professional will explain it clearly.
And if you’re already using hearing aids? Keep them clean. Get them checked yearly. Your hearing doesn’t stop changing-and neither should your care.
Jessica Healey
November 18, 2025 AT 23:04I used to think I was just bad at listening until my audiogram showed a 40dB notch at 4kHz. Turns out I was missing all the s's and t's in conversations. My husband started saying 'I told you' like 3x a day. Now I wear hearing aids and I swear I hear my cat purring from the other room. Life changed.
Levi Hobbs
November 19, 2025 AT 14:33Just want to say: this is one of the most thorough, accurate, and well-structured explanations of audiometry I’ve ever read. Seriously. The breakdown of air vs. bone conduction? The mention of masking and crossover? The reference to ANSI standards? This isn’t just informative-it’s textbook-worthy. Thank you for taking the time to write this.
henry mariono
November 20, 2025 AT 12:27My mom had her first test last year. She was nervous, thought it’d be embarrassing. But the audiologist made it feel like a quiet chat over tea. She got her aids at 52. Now she hears her grandkids say 'I love you' without asking them to repeat it. That’s worth more than any tech gadget.
Sridhar Suvarna
November 20, 2025 AT 19:48Joseph Peel
November 21, 2025 AT 18:26There’s a dangerous myth that hearing loss is just part of aging. It’s not. It’s often preventable. Noise exposure is cumulative. One concert, one power tool, one year of headphones at 80% volume-it adds up. This post is a wake-up call for a generation that thinks earbuds are harmless. We need public health campaigns, not just clinic visits.
Kelsey Robertson
November 22, 2025 AT 01:00Oh please. You're telling me we need to spend $3,000 on 'hearing aids' because we can't hear a whisper? I'm 47 and I hear just fine. I just don't care to listen to people who talk too slow or too loud. This is a scam disguised as medicine. The real issue? Society's decline in conversation quality. We're all just too busy being distracted to pay attention.
Joseph Townsend
November 22, 2025 AT 01:54Bro. I went in for a 'quick check' and came out with a full diagnostic report that looked like a sci-fi alien language. My audiogram had more dips than a rollercoaster at Cedar Point. I thought I was just old. Turns out I’ve been missing my own name for five years. I cried in the parking lot. Then I bought the hearing aids. Best $2,200 I ever spent. My wife kissed me. For real. She said I finally sounded present. That’s not a device. That’s a love potion.
Bill Machi
November 22, 2025 AT 17:39Why are we letting foreign-made audiometers and overpriced American clinics control our health? I’ve seen the data-China and Germany produce better-calibrated devices at 1/3 the cost. And why are we paying audiologists $300/hour when a trained technician with a calibrated phone app can do 90% of the work? This system is broken. It’s profit-driven, not patient-driven. Wake up, America.
Elia DOnald Maluleke
November 24, 2025 AT 11:33There is a metaphysical truth here: hearing is not merely physical. It is the soul's capacity to receive the world's quietest whispers-love, sorrow, truth. When we lose hearing, we do not merely lose decibels; we lose connection. The audiogram is not a chart of frequencies-it is a map of isolation. Let us not wait until silence becomes our only companion.
satya pradeep
November 25, 2025 AT 16:22Prem Hungry
November 25, 2025 AT 19:56Dear friend, you have shared wisdom that can change lives. I am from India, and many here think hearing loss is normal after 50. But I tell my students: your ears are your most delicate sensors. Protect them. Test them. Don’t wait. I have seen young people lose hearing from loud music, and they never recover. Your article is a gift. Thank you for your clarity and care.
Leslie Douglas-Churchwell
November 27, 2025 AT 19:44Let’s be real: audiometry is just the tip of the iceberg. The real conspiracy? Big Pharma and hearing aid corporations have been suppressing natural remedies for decades. Did you know turmeric, magnesium, and ear candling can reverse sensorineural damage? The FDA bans these because they’re unpatentable. Your audiogram? A placebo-driven illusion. Your brain’s neuroplasticity? The only real healer. Wake up. The system is rigged. 🌿👁️🗨️💊