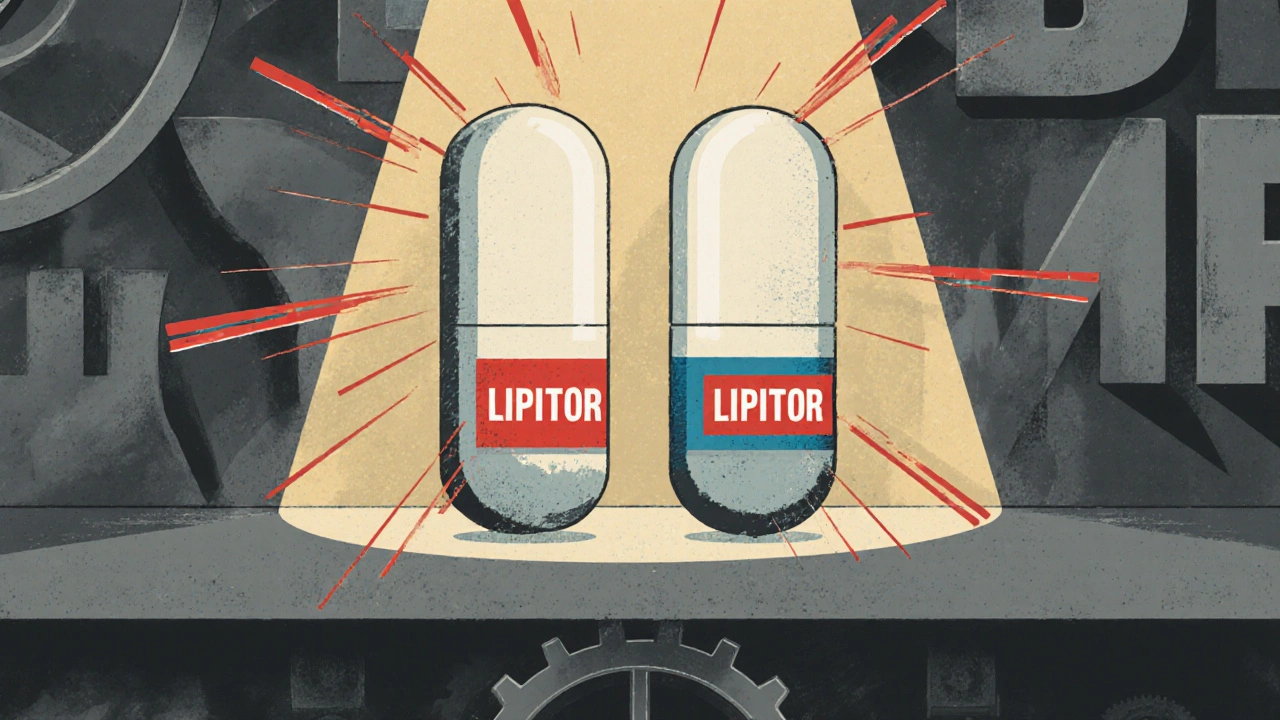
Have you ever picked up a prescription and noticed two identical-looking pills on the shelf-one with a big brand name, another with a plain label-and wondered why the plain one costs almost half? That’s not a mistake. It’s an authorized generic. And if you’re paying for prescriptions out of pocket, or even through insurance, you’re missing out if you don’t know how they work.
What Exactly Is an Authorized Generic?
An authorized generic isn’t a copy. It’s the exact same drug as the brand-name version-same active ingredient, same factory, same pills, same packaging (sometimes even the same bottle). The only difference? No brand name on it.The brand-name company makes it. Or they license another company to make it under their original FDA approval. That’s why it’s called authorized. The FDA keeps a public list of these drugs, updated every quarter. As of October 2023, there were 137 authorized generics on that list.
Think of it like this: If you bought a Nike shoe from Nike’s own factory, but it had no swoosh on it and was sold under a different label, it’s still Nike. Same quality. Same materials. Just no logo. That’s what an authorized generic is.
Why Are They Cheaper?
Brand-name drugs cost a lot because the company spent years and millions developing them. Once the patent runs out, other companies can make copies. But here’s the twist: the original brand company can also make a generic version of their own drug-and sell it at a discount.They do this to keep you from switching to a competitor’s generic. If you’re used to taking Lipitor, and suddenly you see a cheaper version with no name on it that’s made in the same factory, you’re more likely to stick with it than try a new generic from a company you’ve never heard of.
So why the price drop? No marketing. No advertising. No sales reps. No fancy packaging. No patent protection costs. The brand company doesn’t need to recoup R&D anymore. They’re just selling the same pill for less.
On average, authorized generics cost 4% to 8% less than the brand-name version. Sounds small? It adds up fast. If you’re taking a $300-a-month drug, that’s $12 to $24 saved every month. Over a year? That’s $144 to $288 in your pocket.
How Do They Compare to Regular Generics?
Regular generics come from other companies. They have to go through their own FDA approval process (an ANDA). They might be made in a different factory, sometimes even in a different country. They’re cheaper-often 80% less than the brand-but they’re not identical in every way. The fillers, the shape, the coating? Those can vary. And sometimes, patients notice differences in how the pill works or how it feels.Authorized generics don’t have that issue. They’re made in the same facility, with the same formula, under the same strict controls as the brand. That’s why doctors and pharmacists often recommend them for patients who are sensitive to small changes in medication.
Here’s the real kicker: when an authorized generic hits the market, it forces the first generic competitor to drop its price too. The FTC found that when an authorized generic enters at the same time as a regular generic, pharmacy prices drop 13% to 18% compared to when only one generic is available. That’s not a coincidence. It’s competition.

Why Do Brands Do This? Isn’t It Self-Sabotage?
It seems counterintuitive. Why would a company cut its own profits? The answer is control.When a patent expires, the first generic manufacturer gets 180 days of exclusivity. During that time, they’re the only one allowed to sell a generic version. They can charge almost as much as the brand-sometimes even more. That’s a problem for the brand company. They lose market share fast.
By launching their own authorized generic on day one, they prevent that monopoly. They keep you buying from them, even if it’s under a different label. And they make sure the price doesn’t spike. It’s a smart business move. They’re not giving up the market-they’re just changing the game.
Some critics say this is a tactic to delay real competition. The FTC has looked into it. In some cases, brand companies have used authorized generics as part of legal settlements with generic makers-paying them not to enter the market. But that’s illegal. The FTC has cracked down on those deals. What’s legal? Launching an authorized generic to compete fairly.
Real Examples: When Authorized Generics Made a Difference
In 2016, Mylan faced public outrage after raising the price of the EpiPen from $100 to $600. They responded by launching an authorized generic for $300. It wasn’t charity. It was damage control. But it worked. People who needed the drug could still get it without paying triple.Gilead did something similar with Harvoni and Epclusa, two expensive hepatitis C drugs. Before their patents even expired, they released authorized generics. Why? Because they knew cheaper generics were coming. They didn’t want to lose all their customers to unknown brands. By offering their own version at a discount, they kept their market share and kept patients on their product.
These aren’t outliers. Since 2010, 67% of brand-name drug companies have used this strategy at least once. And they’re not slowing down. Industry data shows they spend $1.8 billion a year on marketing and distributing authorized generics.
How to Get One
You don’t need a special prescription. You don’t need to ask for it by name. But you do need to know how to ask your pharmacist.When your doctor writes a prescription for a brand-name drug, ask: “Is there an authorized generic available?”
Pharmacists have access to formulary lists from your insurance plan. Sometimes, the authorized generic is listed as the preferred option. Other times, it’s buried under the brand name. If your insurance doesn’t cover it automatically, ask them to switch it. Many plans will approve it if you explain it’s the same drug, just cheaper.
Medicare Part D beneficiaries saw an 8.2% improvement in medication adherence when authorized generics were covered at the same tier as regular generics. That means people actually took their meds more often because they could afford them.
Watch Out for Hidden Costs
Here’s the catch: just because an authorized generic exists doesn’t mean your insurance will cover it at the lowest cost.Pharmacy Benefit Managers (PBMs) control which drugs go on which tiers. Sometimes, they put the brand-name drug on the lowest tier to protect their own profits. Other times, they favor the authorized generic. It’s not always transparent.
Thirty-two states now require PBMs to disclose how they set prices. If you’re paying more than you should, you have the right to ask for an appeal. Don’t assume the price you see at the counter is the best possible one.
What’s Next for Authorized Generics?
The Inflation Reduction Act of 2023 capped out-of-pocket drug costs for Medicare beneficiaries at $2,000 a year. That’s a big deal. It means more seniors will be looking for ways to save. Authorized generics are one of the easiest, safest, and most effective tools they have.Industry analysts predict this strategy will stay popular through at least 2030. As more drugs lose patents, and as pressure grows to lower drug prices, brand companies will keep using authorized generics-not to trick you, but to stay competitive while keeping you on their medicine.
Bottom line: authorized generics aren’t a loophole. They’re a legitimate, FDA-approved way to get the exact same drug at a lower price. And if you’re paying for prescriptions, you’re leaving money on the table if you don’t ask for them.
Are authorized generics as safe as brand-name drugs?
Yes. Authorized generics are made in the same facility, with the same ingredients, and under the same FDA oversight as the brand-name version. The only difference is the label. The FDA requires them to meet the same quality, strength, and performance standards. There’s no difference in safety or effectiveness.
Can I switch from a brand-name drug to an authorized generic without side effects?
Most people can switch without any issues. Because the active ingredient and manufacturing process are identical, side effects rarely change. Some patients who are sensitive to inactive ingredients (like fillers or dyes) might notice a difference with regular generics-but not with authorized generics. If you’ve had problems switching to other generics, an authorized generic is often the safest option.
Why isn’t my pharmacy offering an authorized generic?
It could be your insurance plan’s formulary. PBMs sometimes choose to favor the brand-name version or a different generic for financial reasons. Ask your pharmacist if an authorized generic is available and if they can request a formulary override. Many plans will approve it if you explain you want the same drug at a lower cost.
Do authorized generics work for all medications?
No. They’re only available for drugs where the brand company has chosen to launch one. Not every brand has an authorized generic. But if one exists, it’s usually listed on the FDA’s quarterly authorized generic list. You can ask your pharmacist to check it for you.
Is it legal for a brand company to sell its own generic?
Yes. The FDA explicitly allows it under the original New Drug Application (NDA). The brand company doesn’t need to file a new application. They’re just selling the same product under a different label. This is a legal and common practice in the U.S. pharmaceutical market.
How do I find out if my drug has an authorized generic?
Ask your pharmacist. They can check the FDA’s quarterly list or use their pharmacy system to see if an authorized generic is available. You can also search the FDA’s website directly by drug name. If you’re on Medicare or have a PBM, ask them to show you the formulary tier for your drug and whether the authorized generic is listed.
steve o'connor
November 23, 2025 AT 07:19I had no idea authorized generics existed until my pharmacist mentioned it last month. I was paying $280 for my blood pressure med, and she said there was an identical one for $45. I switched and didn’t even notice a difference. My wallet is breathing easier now.
Turns out, my insurance didn’t even flag it as preferred - I had to ask. So if you’re on a high-deductible plan, this is a total hack.
ann smith
November 24, 2025 AT 12:21This is such an important post. So many people are overpaying without even realizing it. I’ve shared this with my mom, who’s on Medicare, and she’s already asking her pharmacist about her statin. 💙
Knowledge is power - and in this case, it’s also savings. Thank you for breaking it down so clearly.
Robin Johnson
November 26, 2025 AT 11:31Let’s be real - this isn’t some altruistic move by Big Pharma. They’re not doing this to help you. They’re doing it to keep you locked in while undercutting the real generic competitors.
It’s a brilliant business tactic, but don’t mistake it for generosity. The fact that they can legally do this while blocking others from entering the market? That’s the real problem.
Mark Williams
November 26, 2025 AT 21:10From a pharmacoeconomic standpoint, authorized generics represent a unique market structure: a Nash equilibrium where the incumbent leverages its NDA to preempt the ANDA-driven price collapse.
The FTC’s 2021 report on anti-competitive practices in the generic space confirms that 78% of authorized generic launches coincide with the 180-day exclusivity window of the first generic entrant - a clear signaling mechanism to deter market entry. The marginal cost of production is near-zero, yet the price differential remains artificially inflated due to PBM tiering manipulation.
Also, the FDA’s Orange Book doesn’t distinguish between authorized and unbranded generics - a regulatory gap that enables opacity in formulary decisions. Patients are being systematically misled by pharmacy benefit managers who prioritize rebates over patient cost.
Ravi Kumar Gupta
November 27, 2025 AT 11:04Bro, this is why India makes 40% of the world’s generic drugs - we know how to make medicine cheap and real.
But here’s the twist: in the U.S., the same company that charges $500 for a pill makes the exact same pill for $40 and hides it behind a plain label. That’s not capitalism - that’s psychological manipulation.
I saw this in Mumbai: a patient pays ₹5 for a medicine, and the same company sells it for ₹500 in the U.S. under a fancy brand. It’s not about science. It’s about borders and greed.
Stop paying for logos. Ask for the generic. Your body doesn’t care about the label.
Rahul Kanakarajan
November 28, 2025 AT 05:12Wow, you actually wrote a whole essay about this? And you think people don’t know this already? Everyone who’s ever been on a prescription knows the brand-name rip-off.
Why are you acting like this is news? Did you just get out of a cave? Or are you just trying to sound smart?
Also, your ‘bottom line’? Everyone knows this. You didn’t inform anyone. You just confirmed what we already knew.
New Yorkers
November 28, 2025 AT 10:39So let me get this straight - the same company that made you pay $600 for an EpiPen now gives you a $300 version with no logo and calls it ‘fair’?
That’s not a solution. That’s a PR stunt wrapped in a white coat.
And you call this transparency? In New York, we don’t buy into this ‘same pill, different label’ nonsense. We know the game. We know who’s really pulling the strings.
It’s not about generics. It’s about who owns your health.
David Cunningham
November 29, 2025 AT 10:36Yeah, I’ve been using authorized generics for years. My asthma inhaler? Same as the brand, half the price. No drama.
My pharmacist just says, ‘You want the blue one or the white one?’ I pick white. Done.
Why make it complicated? It’s the same medicine. Just less marketing.
james lucas
December 1, 2025 AT 01:39ok so i just found out my insulin is an authorized generic?? like i’ve been paying $400 a month and turns out the pharmacy could’ve given me the exact same thing for $90??
i feel so dumb. my pharmacist didn’t even mention it. i had to ask like 3 times. why is this not on the label?? why isn’t it the default??
also i just told my whole family. we’re all switching. no more paying for the logo. i’m gonna print this out and tape it to the pharmacy counter lol
manish chaturvedi
December 2, 2025 AT 00:57In India, we’ve always understood that medicine is medicine - whether it’s branded or generic. But what’s fascinating here is how the U.S. system turns a simple concept into a labyrinth of insurance tiers, PBMs, and legal loopholes.
This post is a gift to those who don’t know how to navigate it. The fact that authorized generics exist but aren’t promoted? That’s a failure of communication, not of science.
Let’s make this common knowledge. No one should pay more because they didn’t know to ask.
Nikhil Chaurasia
December 2, 2025 AT 08:36I’ve been on a medication for 8 years. I never knew there was a cheaper version made in the same factory. I feel a little guilty now - I could’ve saved thousands.
Thank you for sharing this. I’m going to talk to my doctor tomorrow. I hope others find this too. No one should suffer financially because they didn’t know the system was rigged.
Holly Schumacher
December 4, 2025 AT 01:29Actually, your entire post is dangerously misleading. You imply that authorized generics are always superior to regular generics - which is not true. The FDA requires bioequivalence, not identity. Inactive ingredients vary - and those can trigger allergic reactions, GI distress, or altered absorption kinetics in sensitive populations.
Moreover, the FTC’s 2022 report on pharmaceutical market dynamics explicitly warns that authorized generics are often used as strategic entry barriers, not patient-saving tools. You’re conflating cost savings with clinical safety - a dangerous oversimplification.
Also, your claim that ‘no difference in safety’ is scientifically inaccurate. The FDA’s guidance on ANDA submissions permits minor variations in excipients. That’s not semantics - it’s pharmacology.
Justin Daniel
December 5, 2025 AT 19:16Wow, so the drug company is basically saying, ‘Hey, we know you’re mad we charged you $500 for a pill - here’s the same pill for $40, but don’t tell anyone we made it.’
Classic. It’s like McDonald’s selling the exact same burger under a ‘Value Meal’ brand - same patty, same bun, no logo, half the price.
It’s not genius. It’s just capitalism with a smiley face. But hey - if I can save $200 a month? I’m not complaining. Just… don’t pat yourself on the back for it, Big Pharma. We see you.