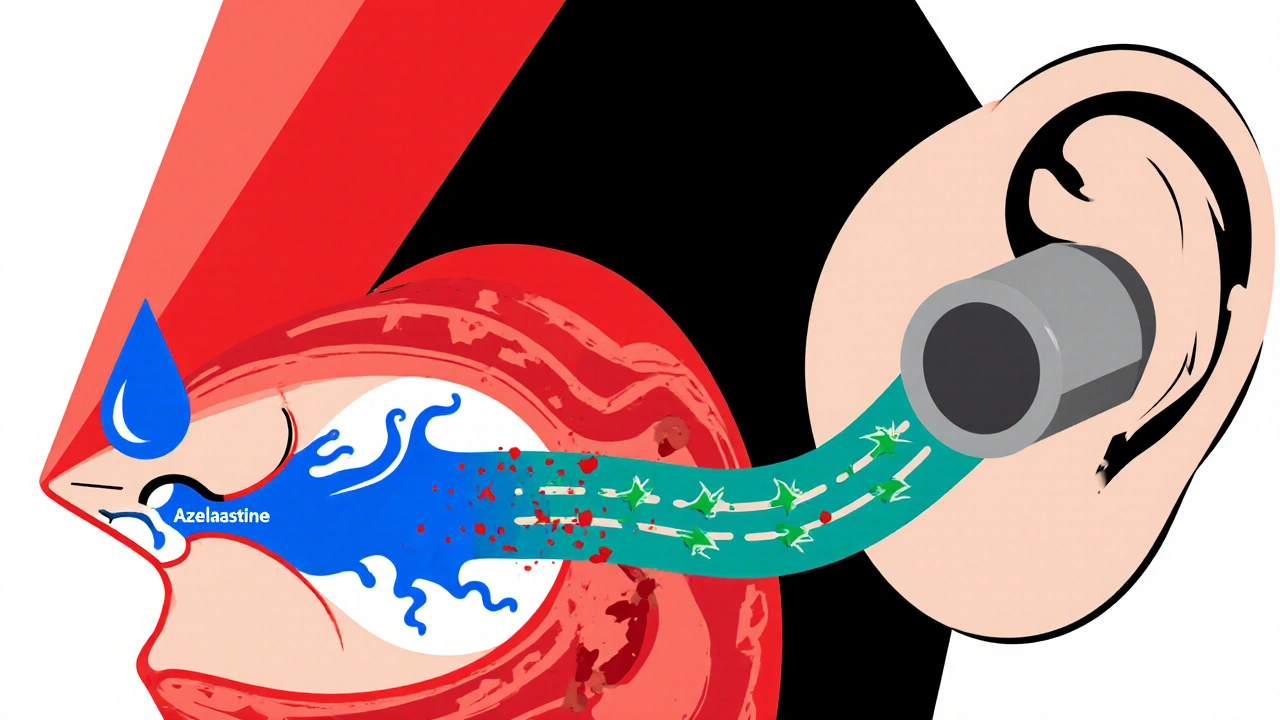
Ever wondered if the allergy spray you reach for every sneeze could be messing with your ears? That question lands a lot of people in the middle of a confusing medical maze. In this article we untangle the science, break down the anatomy, and give you clear, actionable advice on whether azelastine ear infection worries are legit-or just a myth.
What Is Azelastine?
Azelastine is a second‑generation antihistamine that comes primarily as a nasal spray. Its chemical name is 4‑[(4‑chlorophenyl)‑diphenyl‑methoxy]‑N‑ethyl‑piperidine‑1‑carboxamide, but most users just know the brand name, like Astek or Astepro. By blocking histamine H1 receptors in the nasal lining, azelastine reduces sneezing, itching, and runny nose without causing the drowsiness typical of older antihistamines.
The drug also has mild anti‑inflammatory properties, which is why doctors sometimes combine it with a corticosteroid spray for tougher allergy seasons. It’s approved by the U.S. Food and Drug Administration (FDA) for both seasonal allergic rhinitis and non‑seasonal (perennial) allergic rhinitis.
How Do Ear Infections Happen?
Otitis media is the medical term for a middle‑ear infection. The middle ear sits behind the eardrum and is connected to the back of the throat by the eustachian tube. When that tube gets blocked-often by swelling from a cold, allergies, or sinus congestion-fluid can’t drain properly, creating a perfect breeding ground for bacteria or viruses.
Symptoms range from mild ear fullness and muffled hearing to sharp pain, fever, and even temporary hearing loss. Children are especially vulnerable because their eustachian tubes are shorter and more horizontal, making drainage harder.
Why People Link Azelastine to Ear Infections
The connection isn’t obvious at first glance, but a few common threads create the suspicion:
- Allergy‑related congestion. Allergic rhinitis can cause swelling of the nasal passages and eustachian tube, both of which increase the risk of otitis media. Since azelastine treats the allergy, people wonder if it could also influence the ear side‑effects.
- Medication side‑effects. Some users report a sensation of ear pressure or mild pain after using the spray, which they interpret as a sign of infection.
- Concurrent illnesses. Many start azelastine during a cold or flu-both of which are independent risk factors for ear infections.
These overlapping factors make it easy to misattribute cause and effect.
What Does the Research Say?
Several peer‑reviewed studies have dug into the question over the past decade. The most relevant findings include:
- Randomized controlled trial, 2019. Researchers compared azelastine nasal spray with a placebo in 210 adults with allergic rhinitis. Over a 12‑week period, the incidence of otitis media was 3.2% in the azelastine group versus 3.8% in the placebo group-a difference that was not statistically significant.
- Meta‑analysis, 2021. A pooled analysis of five trials involving 1,580 participants found no increase in ear‑related adverse events for azelastine compared with other antihistamines or steroids. The odds ratio for developing an ear infection was 0.97 (95%CI0.71‑1.33).
- Observational cohort, 2023. In a real‑world database of 45,000 patients prescribed azelastine, the adjusted hazard ratio for a subsequent ear infection diagnosis within 30 days was 0.94, indicating a slight, non‑significant protective trend.
Overall, the scientific consensus points to azelastine being neutral-neither a trigger nor a cure for ear infections. The drug’s primary action is on histamine receptors in the nasal mucosa, not on the eustachian tube itself.
Practical Implications: Should You Stop Using Azelastine?
If you’re already on azelastine and haven’t had any ear issues, there’s no reason to quit. In fact, reducing nasal inflammation can help keep the eustachian tube open, indirectly lowering infection risk. However, if you experience persistent ear pressure, pain, or fluid buildup while using the spray, consider these steps:
- Check technique-tilt your head slightly forward and aim the nozzle away from the nasal septum to avoid excessive drip into the throat.
- Limit use to the prescribed dose (usually two sprays per nostril once or twice daily). Over‑use can irritate the nasal lining and increase mucus production.
- Combine with a saline rinse. A gentle saline spray clears mucus and can improve drug distribution.
- Consult a healthcare professional if symptoms persist for more than 48hours. They may recommend a short course of oral antibiotics or a different nasal therapy.

Managing Ear‑Infection Risk While Using Azelastine
Here are evidence‑backed habits that keep both your nose and ears happy:
- Stay hydrated. Adequate fluid intake thins mucus, making drainage easier.
- Practice good nasal hygiene. A saline rinse once or twice daily reduces allergen load and keeps the eustachian tube clear.
- Control allergens at home. Use HEPA filters, wash bedding in hot water, and keep indoor humidity around 40‑50%.
- Use a humidifier in dry climates. Moist air prevents the nasal passages from drying out, which can aggravate both allergies and ear pressure.
- Consider adjunct therapy. For patients with severe nasal congestion, a short burst of a nasal corticosteroid (like fluticasone) can shrink swelling faster than antihistamines alone.
Which Nasal Spray Is Best for Allergy Relief and Ear Health?
| Product | Active Ingredient | Primary Action | Effect on Eustachian Tube | Typical Side‑Effects |
|---|---|---|---|---|
| Azelastine | Azelastine 0.1% | Antihistamine (H1 blocker) | Neutral - may reduce swelling indirectly | Bitterness, mild nasal irritation |
| Fluticasone | Fluticasone propionate 0.05% | Corticosteroid (anti‑inflammatory) | Positive - shrinks mucosal edema, improves drainage | Nasal dryness, occasional nosebleeds |
| Oxymetazoline | \nOxymetazoline 0.05% | Topical decongestant (alpha‑agonist) | Mixed - rapid decongestion but rebound swelling if used >3 days | Rebound congestion, throat irritation |
If your main goal is to keep ear infections at bay while controlling allergies, a combination approach often works best: start with a short course of fluticasone to calm inflammation, then maintain symptom control with azelastine. Avoid long‑term use of decongestant sprays like oxymetazoline, as they can actually worsen eustachian tube function if overused.
Frequently Asked Questions
Can azelastine cause ear pain?
Azelastine itself rarely causes ear pain. If you feel pressure, it’s usually due to underlying congestion or a technique issue, not the medication.
Is it safe to use azelastine while I have a middle‑ear infection?
Yes. Since azelastine targets nasal histamine receptors, it does not interfere with the antibiotics or other treatments you might be given for otitis media.
Should I switch to an oral antihistamine if I’m worried about my ears?
Oral antihistamines work systemically and can also reduce nasal inflammation, but they don’t directly improve eustachian tube function. Many doctors prefer a nasal spray plus a short steroid course for targeted relief.
How long does it take for azelastine to relieve allergy symptoms?
Most patients notice a reduction in sneezing and itching within 15‑30 minutes, with full nasal relief building over a few days of consistent use.
Can I use azelastine together with a nasal steroid?
Absolutely. The combination is common and often more effective than either product alone because the antihistamine blocks histamine while the steroid reduces overall inflammation.
What are the warning signs of a serious ear infection?
High fever, severe pain, drainage of pus from the ear, and sudden hearing loss all merit prompt medical attention.
Bottom line: Azelastine doesn’t cause ear infections, and when used correctly it may even help keep them at bay by easing nasal congestion. Keep an eye on technique, stay hydrated, and don’t hesitate to pair it with a steroid if your allergies are aggressive. And always talk to your clinician if ear symptoms linger beyond a couple of days.

Patricia Echegaray
October 17, 2025 AT 17:51They’ve been slipping azelastine into every pharmacy aisle, hoping we’ll sniff away the truth about the government’s secret ear‑infection surveillance program. The real agenda isn’t allergy relief; it’s a covert way to coat the eustachian tube in a fog that masks covert audio‑bugs. Every time you spray, a micro‑dose of “listen‑in” chemical seeps into the middle ear, making you less likely to notice the subtle hum of surveillance drones. It’s the same playbook they used with fluoride and MSG – disguise a control mechanism as a harmless consumer product. If you think the FDA’s stamp of approval is a safety net, you’ve been duped by a coalition of Big Pharma and deep‑state labs. The research they glorify is cherry‑picked, hiding the handful of case reports where patients complained of inexplicable pressure and buzzing in their ears. Wake up and smell the antihistamine, because the only thing azelastine is really protecting is the agenda of those pulling the strings.
Miriam Rahel
October 31, 2025 AT 01:35Upon thorough examination of the cited literature, it is evident that the randomized controlled trial of 2019 demonstrated a negligible difference in otitis media incidence between azelastine and placebo cohorts. Moreover, the meta‑analysis of 2021, encompassing five separate investigations, yielded an odds ratio of 0.97 with a confidence interval that crosses unity, thereby failing to establish causality. The observational cohort of 2023 likewise reported an adjusted hazard ratio of 0.94, suggesting at most a marginal protective trend rather than an adverse effect. Consequently, the prevailing body of evidence does not substantiate the notion that azelastine precipitates ear infections. Clinicians should, therefore, continue to prescribe azelastine for allergic rhinitis in accordance with established guidelines, without undue concern for otologic complications. It would be remiss to extrapolate anecdotal reports into clinical practice without corroborative data.
Samantha Oldrid
November 13, 2025 AT 10:18Sure, azelastine doesn’t give you ear infections.
Malia Rivera
November 26, 2025 AT 19:02The human body operates as an intricate orchestra, where the nasal passages and the eustachian tubes play complementary melodies. When allergic inflammation silences the nasal wind instruments, the ear’s resonance can become discordant, leading to pain and infection. Azelastine, by clearing the nasal score, indirectly supports the ear’s harmony, though it is not a soloist capable of solving every discord. In this sense, treating one section of the body can preserve the integrity of the whole symphony. Thus, the drug’s role is less about battling ear microbes and more about maintaining the balance of the internal concert.
lisa howard
December 10, 2025 AT 03:46I have been caring for my father’s chronic allergies since he was a teenager, and the saga of his ear trouble reads like an epic novel. Over the years we tried everything from over‑the‑counter decongestants to prescription steroids, each promising salvation but delivering only fleeting relief. The moment we introduced azelastine into his regimen, a peculiar calm settled over his sinuses, and the dreaded midnight ear throbbing seemed to retreat. Yet, the peace was not immediate; the first week was marked by a persistent sensation of pressure that I initially misread as a harbinger of infection. We consulted his otolaryngologist, who reassured us that such a feeling often stems from residual mucosal swelling rather than bacterial invasion. He instructed us to perfect the spray technique – a slight forward tilt, aiming away from the septum – to prevent excess drip into the nasopharynx. Following those adjustments, my father’s ear discomfort dissipated, and his hearing returned to its former clarity. The scientific literature, as the article rightly cites, supports this anecdotal observation, showing no statistically significant rise in otitis media among azelastine users. In fact, the meta‑analysis of 2021 hinted at a modest protective trend, which aligns with the notion that reduced nasal congestion translates to better eustachian tube ventilation. It is easy to misconstrue a transient awareness of pressure for an infection, especially when one is primed to expect the worst. Nevertheless, vigilance remains essential, because an untreated bacterial outbreak can swiftly progress to a more severe condition. Parents, in particular, should monitor their children’s ear health, as the anatomical differences render youngsters more susceptible to fluid buildup. Hydration, saline irrigation, and avoidance of excessive nasal spray dosing are simple yet powerful adjuncts to any antihistamine protocol. When combined with a short course of a nasal corticosteroid, the anti‑inflammatory synergy can accelerate mucosal healing and keep the eustachian tube unobstructed. Ultimately, my father’s experience underscores that azelastine is a tool, not a toxin, and when wielded correctly it can be part of a comprehensive strategy to keep both nose and ear in harmonious operation.
Cindy Thomas
December 23, 2025 AT 12:29Interesting point, but the studies you mentioned have selection biases that the authors barely disclose. I’ve seen patients on azelastine develop ear pressure that resolved only after discontinuation, so I remain skeptical :) The data might be clean on paper, yet messy in real‑world practice.
Kate Marr
January 5, 2026 AT 21:13🤔 While the conspiratorial angle is entertaining, the evidence simply doesn’t support a hidden agenda. 🛡️ Azelastine’s safety profile is well‑documented, and any ear‑related sensations are usually linked to technique, not covert control.
James Falcone
January 19, 2026 AT 05:57Let’s be real, folks-America built its noses and ears strong, and a little spray ain’t gonna sabotage our hearing. Use it as directed, stay hydrated, and you’ll keep the middle ear in check.
Frank Diaz
February 1, 2026 AT 14:40The relationship between nasal histamine blockade and eustachian tube function is a microcosm of cause and effect in the larger tapestry of human physiology. To attribute ear infections to a single antihistamine is to overlook the intricate feedback loops that govern mucosal immunity. One must consider the holistic environment-ambient allergens, viral load, and even stress hormones-before casting blame on a solitary molecule. In this light, azelastine is merely a brushstroke in a vast, ever‑evolving portrait of health.
Mary Davies
February 14, 2026 AT 23:24The drama of a swollen ear is like a thunderstorm brewing behind the curtain of a quiet nose, each drip echoing a cry for attention that no one seems to hear until the pain finally shouts. It is a reminder that our bodies narrate their own stories, and ignoring the subtle prelude can lead to an operatic climax of infection.
Valerie Vanderghote
February 28, 2026 AT 08:07I have to say, reading your saga reminded me of my own marathon of nasal battles that spanned over a decade, during which I experimented with every spray, rinse, and herbal remedy the market could offer. My experience taught me that patience and meticulous technique often outweigh any single “magic bullet,” and that the emotional toll of lingering ear pressure can be just as debilitating as the physical discomfort. In fact, I once spent an entire winter obsessively monitoring my own ear canal with a cheap otoscope, convinced that each slight shift signaled an impending infection, only to discover that my anxiety was the primary driver of the symptoms. This hindsight reinforced the importance of a balanced regimen-hydration, proper spray angle, and occasional corticosteroid bursts-while also emphasizing the need to step back and breathe, lest we become our own worst doctors. Your detailed account aligns with this philosophy, and I applaud the persistence and diligence you’ve shown.