Understanding Parkinson's Disease in the Elderly
As we age, our bodies undergo numerous changes, and one of the most common challenges faced by older adults is the development of neurological disorders. Among these, Parkinson's Disease (PD) is a prevalent condition that affects millions of people worldwide. PD is a progressive neurodegenerative disorder that primarily affects the elderly population.
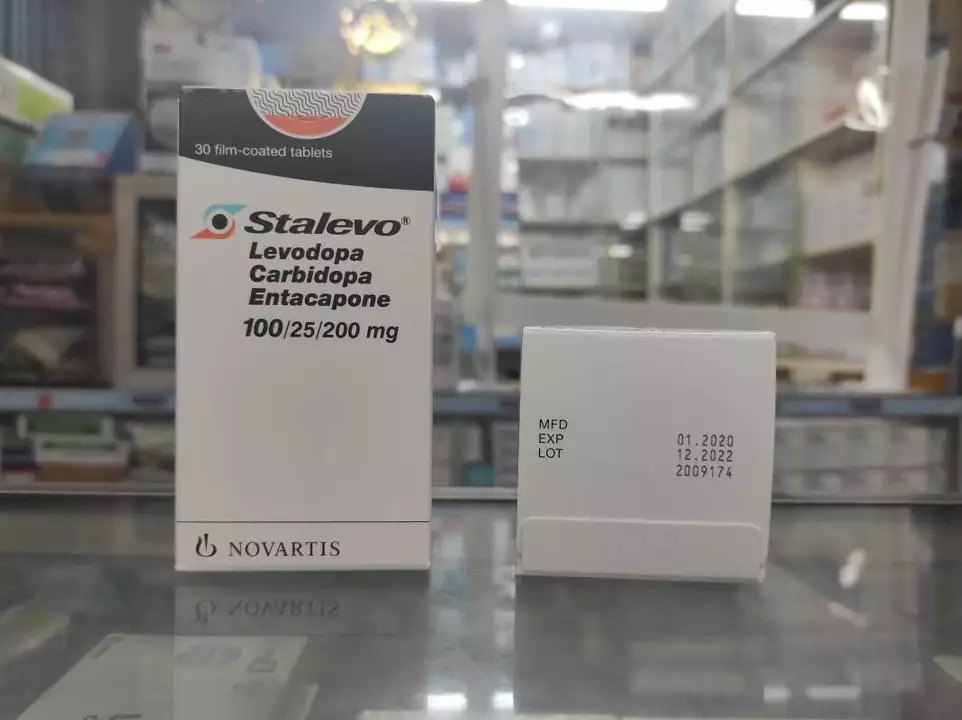
In this article, we will explore the role of Carbidopa-Levodopa in managing the symptoms of Parkinson's Disease in older adults and discuss the special considerations that need to be taken into account when treating geriatric Parkinson's patients.
Carbidopa-Levodopa: The Gold Standard for Parkinson's Treatment
Carbidopa-Levodopa is a combination medication that is widely considered the gold standard treatment for Parkinson's Disease. Levodopa is a precursor to dopamine, which is the neurotransmitter that is deficient in PD patients. When taken orally, Levodopa crosses the blood-brain barrier and is converted into dopamine, thereby replenishing the levels of this neurotransmitter and improving motor symptoms.
Carbidopa, on the other hand, is a peripheral decarboxylase inhibitor. It prevents the breakdown of Levodopa in the bloodstream, ensuring that more Levodopa reaches the brain and is converted into dopamine. This combination not only increases the efficacy of Levodopa but also helps reduce the side effects associated with its use.
Special Considerations for Geriatric Parkinson's Patients
While Carbidopa-Levodopa has proven to be an effective treatment for PD, it is essential to consider the unique challenges and needs of geriatric patients. Older adults often have multiple comorbidities and may be taking several medications, which can affect the absorption, metabolism, and clearance of Carbidopa-Levodopa. Moreover, the presence of other age-related issues such as cognitive decline, balance problems, and increased sensitivity to side effects can impact the overall effectiveness of the treatment.
In the following sections, we will discuss some of the key concerns and special considerations that should be taken into account when treating elderly Parkinson's patients with Carbidopa-Levodopa.
1. Starting with a Low Dose and Titrate Slowly
One of the primary concerns for geriatric patients is their increased sensitivity to the side effects of medications. To minimize the risk of adverse effects, it is recommended to start Carbidopa-Levodopa therapy with a low dose and slowly titrate the dosage upwards as needed. This slow titration allows the patient's body to adjust to the medication and helps identify the optimal dose that provides symptom relief without causing significant side effects.
Moreover, regular monitoring and follow-ups with the healthcare provider are crucial during the titration phase to assess the patient's response to the treatment and make any necessary adjustments to the dosage regimen.
2. Monitoring for Side Effects
Geriatric patients are more susceptible to the side effects of Carbidopa-Levodopa, which may include nausea, vomiting, orthostatic hypotension, and hallucinations. It is essential to educate patients and their caregivers about these potential side effects and encourage them to report any symptoms to their healthcare provider.
In some cases, additional medications may be prescribed to manage these side effects, such as antiemetics for nausea and anticholinergic agents for hallucinations. Periodic assessments of the patient's overall health and medication regimen can help identify any side effects and optimize the treatment plan accordingly.
3. Managing Drug Interactions
Older adults are often on multiple medications due to various comorbidities, which can increase the risk of drug interactions. Some medications can interfere with the absorption or metabolism of Carbidopa-Levodopa, leading to reduced efficacy or increased side effects. For example, antacids and iron supplements can bind to Levodopa and reduce its absorption, while certain antidepressants and antipsychotics can exacerbate the motor symptoms of PD.
It is crucial to review the patient's medication list regularly and make any necessary adjustments to minimize the risk of drug interactions. In some cases, alternative medications or treatment approaches may be considered to ensure optimal management of the patient's health.
4. Addressing Cognitive and Psychiatric Issues
Geriatric patients with Parkinson's Disease may also experience cognitive decline and psychiatric symptoms such as depression, anxiety, and hallucinations. These issues can impact the patient's quality of life and their ability to adhere to the treatment regimen. It is essential to assess and address these concerns in conjunction with the Carbidopa-Levodopa therapy.
Cognitive and psychiatric symptoms may be managed through medications, counseling, or non-pharmacological interventions such as cognitive-behavioral therapy, support groups, and caregiver education. A comprehensive and holistic approach to treatment can help improve the patient's overall well-being and enhance their response to Carbidopa-Levodopa therapy.
5. Considering Alternative Treatment Options
While Carbidopa-Levodopa is the cornerstone of Parkinson's Disease treatment, it may not be suitable for all geriatric patients. In cases where Carbidopa-Levodopa is not well-tolerated or contraindicated due to drug interactions or comorbidities, alternative treatment options may be considered.
These may include other dopaminergic medications, such as dopamine agonists, catechol-O-methyltransferase (COMT) inhibitors, or monoamine oxidase-B (MAO-B) inhibitors. Additionally, non-pharmacological interventions such as physical therapy, occupational therapy, and speech therapy can play a crucial role in managing the symptoms of PD and improving the patient's quality of life.
Conclusion
Treating geriatric patients with Parkinson's Disease requires special consideration and a tailored approach to ensure optimal symptom management and quality of life. Carbidopa-Levodopa remains the gold standard treatment for PD, but healthcare providers must be aware of the unique challenges faced by older adults and adapt the treatment plan accordingly. By addressing issues such as side effects, drug interactions, cognitive decline, and psychiatric symptoms, we can provide comprehensive care for geriatric Parkinson's patients and help them maintain their independence and well-being.
Nawal Albakri
May 7, 2023 AT 13:31Megan Oftedal
May 8, 2023 AT 02:44Musa Aminu
May 9, 2023 AT 19:05robert maisha
May 11, 2023 AT 05:22Alexander Ståhlberg
May 11, 2023 AT 10:39Robert Andersen
May 12, 2023 AT 09:28Eric Donald
May 12, 2023 AT 16:43Brenda Flores
May 13, 2023 AT 07:26Jackie R
May 14, 2023 AT 02:58Josh Arce
May 14, 2023 AT 21:58Eli Grinvald
May 15, 2023 AT 15:26Alexis Hernandez
May 17, 2023 AT 01:00brajagopal debbarma
May 18, 2023 AT 05:40