Steroid Eye Risk Assessment Tool
This tool estimates your risk of developing steroid-induced eye conditions based on the information you provide. Remember: this is for educational purposes only. Always consult your eye doctor for medical advice.
Steroid Exposure
Your Risk Factors
Your Risk Level
When you're on steroids for asthma, rheumatoid arthritis, or a skin condition, your body gets relief. But your eyes? They might be paying a hidden price. Long-term steroid use - whether it’s pills, injections, inhalers, or eye drops - can quietly trigger two serious eye problems: cataracts and glaucoma. And here’s the scary part: you might not feel a thing until it’s too late.
How Steroids Turn Your Eyes Into a Risk Zone
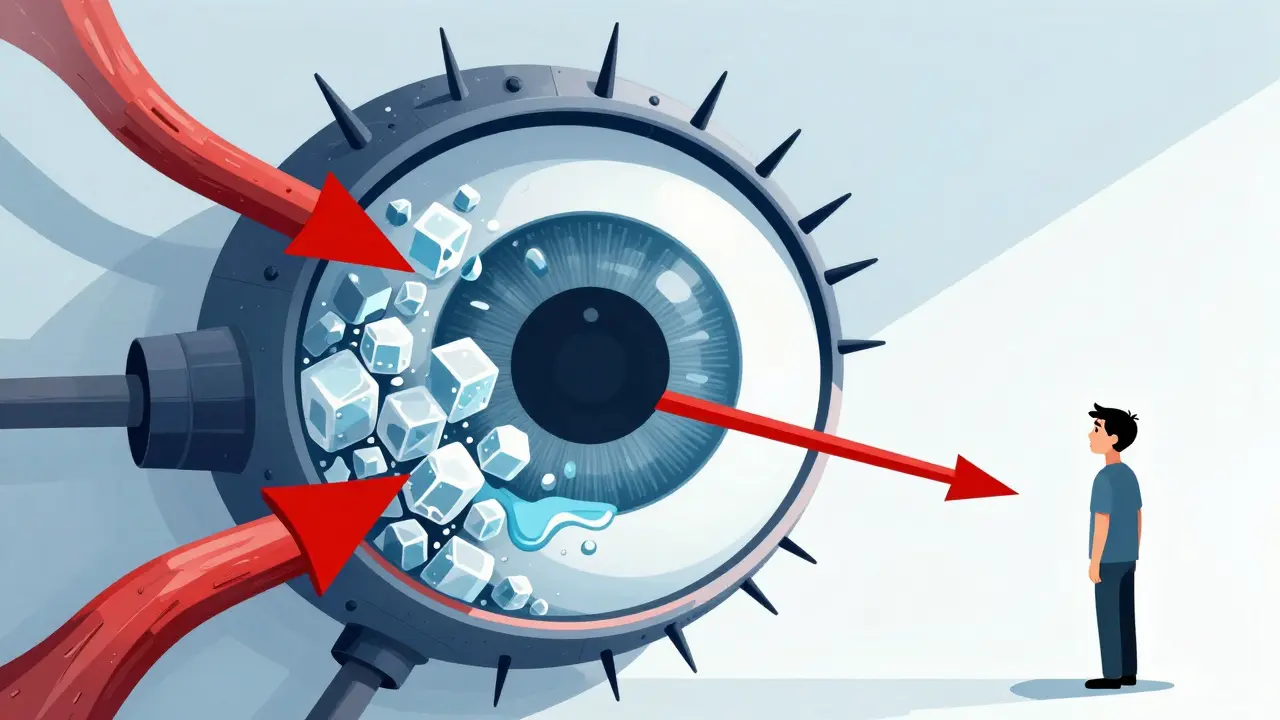
Steroids don’t just calm inflammation. They change how your eye works from the inside out. For cataracts, the problem starts with the lens. Normally, your lens stays clear. But when steroids hang around too long, they bind to proteins in the lens and form strange, stable chemical bonds called Schiff base adducts. These don’t happen in regular age-related cataracts. They’re unique to steroid use. The result? A cloudy patch forms right at the back of the lens - called a posterior subcapsular cataract. This kind doesn’t just blur your vision slowly. It can wreck your ability to see in bright light, make halos around headlights at night, and make colors look washed out - all within weeks or months.Glaucoma: The Silent Thief of Vision
Glaucoma from steroids works differently. It’s not about the lens - it’s about pressure. Your eye makes fluid (aqueous humor) and drains it through a mesh-like channel. Steroids clog that drain. When drainage slows, pressure builds. That’s called intraocular pressure (IOP). High IOP crushes the optic nerve over time. Once that nerve dies, vision loss is permanent. And here’s what most people don’t know: not everyone reacts the same way. About 5% of people are high responders - their IOP spikes dangerously with even short steroid use. Another 25-30% are moderate responders. That means nearly one in three people on steroids could be at risk. And if you already have glaucoma? You’re almost guaranteed to be a responder. Studies show up to 90% of glaucoma patients see their eye pressure climb with steroid exposure.Who’s Most at Risk?
Some people are walking time bombs for steroid eye damage. You’re at higher risk if:- You have a family history of glaucoma
- You’ve been diagnosed with glaucoma already
- You’re using steroid eye drops daily for more than 2-4 weeks
- You’ve had cataract surgery recently - steroid drops are common after, and that’s when glaucoma often strikes
- You’re on oral steroids like prednisone for more than a month
Here’s the twist: nearly 35% of steroid-induced glaucoma cases happen in people with no prior eye problems. No warning. No symptoms. Just sudden vision loss.
How Fast Does It Happen?
Timing matters. Steroid-induced cataracts can start forming in as little as 2-4 weeks of daily steroid eye drops. Oral steroids take longer - usually 3-6 months - but the damage still happens. Glaucoma can creep up even faster. One patient in Toronto told his doctor he’d been using steroid drops for uveitis for five months. He thought his eyes felt better. Turns out, his IOP had jumped 18 mmHg. He’d already lost 20% of his peripheral vision. By the time he noticed tunnel vision, it was too late to reverse.Not all pressure spikes are equal. Research shows:
- 66% of users see IOP rise by less than 5 mmHg - usually harmless
- 30% get a rise of 6-15 mmHg - needs monitoring
- 5% spike over 15 mmHg - high risk for nerve damage
And here’s the good news: if caught early, the pressure usually drops back to normal when you stop the steroid. But if the optic nerve is already damaged? That’s permanent.
Topical Drops Are the Biggest Threat
Not all steroid routes are equal. Eye drops are the most dangerous for your eyes because they’re applied directly. A single drop can deliver 100 times more steroid to your eye than an oral pill. That’s why patients using steroid eye drops for months - even for mild inflammation - are the most likely to develop cataracts or glaucoma. Oral steroids still pose a risk, but you need longer exposure. Inhaled steroids? Lower risk, but still possible if used daily for years. Injectable steroids? Rarely cause eye issues unless given repeatedly near the eye.What Symptoms Should You Watch For?
Steroid glaucoma is silent. No pain. No redness. No warning. That’s why it’s called the “silent thief.” But cataracts? They’re harder to ignore:- Blurry vision that doesn’t improve with glasses
- Seeing halos or glare around lights, especially at night
- Colors look faded or yellowed
- Needing brighter light to read
- Frequent changes in your eyeglass prescription
If you’re on long-term steroids and notice any of these, don’t wait. Get your eyes checked - now.
How Doctors Monitor for Damage
The American Academy of Ophthalmology has clear rules. If you’re going on steroids for more than two weeks, you need an eye exam before you start. Then:- First check: 2 weeks after starting
- Second check: 4-6 weeks after starting
- Third check: 3 months in
- After that: every 6 months if pressure is normal
Each visit includes measuring your eye pressure and checking your optic nerve. No shortcuts. No skipping. Yet, studies show only 42% of primary care doctors refer their patients for this. That’s a gap. If your doctor didn’t mention an eye exam, ask. Don’t assume they know.
What Can You Do to Protect Your Vision?
You can’t always avoid steroids. But you can control how you use them:- Use the lowest dose possible. More isn’t better. It’s riskier.
- Shorten the duration. If you’re on steroid drops for more than 4 weeks, talk to your doctor about switching.
- Ask about safer alternatives. Loteprednol etabonate is a newer steroid with much lower risk of IOP spikes. It’s now recommended for long-term use in many cases.
- Know your family history. If glaucoma runs in your family, tell your eye doctor before starting steroids.
- Get regular eye exams. Every six months during treatment. Even if you feel fine.
One patient in Toronto, on prednisone for asthma, didn’t think eye exams were needed. After six months, her vision dropped to 20/80. She had advanced cataracts. She needed surgery. “I thought the steroids were helping me breathe,” she said. “I didn’t know they were blinding me.”
What Happens If It’s Too Late?
If you’ve already developed steroid-induced cataracts, surgery can fix them. It’s safe, common, and usually restores vision. But if glaucoma has damaged your optic nerve? There’s no cure. You’ll need lifelong eye drops, laser treatments, or even surgery just to slow further loss. The goal? Preserve what’s left. That’s why early detection isn’t optional - it’s your only defense.The Bigger Picture
In 2023, over 12 million steroid eye drop prescriptions were filled in the U.S. alone. Millions more took oral steroids. The CDC estimates 3.1 million Americans use systemic steroids long-term. That’s a lot of people at risk. And while newer steroid alternatives are emerging, many doctors still reach for the old, cheap, powerful ones. The FDA and EMA both require warning labels on steroid products - but warnings don’t stop damage. Awareness does.Research is moving fast. In 2024, scientists identified genetic markers that predict who’s likely to be a steroid responder with 85% accuracy. Soon, a simple blood test might tell you if you’re at high risk before you even start treatment. Tele-ophthalmology programs are already helping Veterans Health Administration patients monitor eye pressure at home. But until those tools are everywhere, the best protection is still you - asking questions, showing up for exams, and refusing to ignore the signs.
Final Warning
Steroids save lives. But they don’t care about your eyes. If you’re on them long-term, your eyes need their own plan. Don’t wait for blurry vision. Don’t wait for tunnel vision. Schedule that eye exam. Ask your doctor about alternatives. Know your numbers. Your vision isn’t something you can afford to gamble with.Can steroid eye drops cause glaucoma even if I don’t have a history of it?
Yes. Nearly 35% of steroid-induced glaucoma cases happen in people with no prior eye problems. You don’t need a family history or previous diagnosis to be at risk. Any long-term use of steroid eye drops - even for mild inflammation - can raise eye pressure enough to damage the optic nerve over time.
How long do I need to use steroids before eye damage starts?
For steroid eye drops, damage can begin in as little as 2-4 weeks. Oral steroids usually take longer - around 3-6 months - but the risk still builds over time. The longer you use them, the higher your chance of developing cataracts or glaucoma. That’s why doctors recommend checking eye pressure after just two weeks of use.
Is steroid-induced glaucoma reversible?
The high eye pressure caused by steroids usually goes down after you stop the medication. But if the pressure stayed high long enough to damage your optic nerve, that damage is permanent. That’s why early detection is critical - you can save your vision if you catch it before the nerve is harmed.
Are there safer steroid alternatives for the eyes?
Yes. Loteprednol etabonate is a newer steroid designed to break down quickly in the eye, reducing the risk of pressure spikes. Studies show it causes significantly less IOP elevation than older steroids like prednisolone. If you need long-term treatment, ask your eye doctor if this option is right for you.
Should I stop my steroids if I’m worried about my eyes?
Never stop steroids without talking to your doctor. Stopping suddenly can cause serious health problems. Instead, get your eyes checked. If pressure is rising, your doctor can adjust your treatment - maybe lower the dose, switch to a safer steroid, or add pressure-lowering eye drops. The goal is to protect both your overall health and your vision.
How often should I get my eyes checked while on steroids?
If you’re on steroids for more than two weeks, get a baseline eye exam before starting. Then: at 2 weeks, 4-6 weeks, and 3 months. If your pressure stays normal, continue every 6 months. If you’re a high-risk patient - like someone with glaucoma or a family history - your doctor may recommend checks every 3 months.

Ajay Brahmandam
December 21, 2025 AT 14:35Been on steroid eye drops for uveitis for 6 months. No symptoms, but I got my pressure checked every 8 weeks like the doc said. Turned out my IOP was at 28. Scared the hell out of me. Now I’m on loteprednol and my numbers are back to 14. Don’t wait until you can’t see street signs. Get checked.
Johnnie R. Bailey
December 23, 2025 AT 04:18It’s wild how medicine keeps giving us tools that heal one part of us while quietly breaking another. Steroids are like a silent partner in your body-helpful, powerful, but never really honest about the cost. We fix asthma, we fix inflammation, we fix pain… and then one day, the world goes blurry and we realize we forgot to ask the eyes if they were okay.
Maybe the real disease isn’t the condition we’re treating-it’s the assumption that healing one system doesn’t require checking on all of them.
I’ve seen patients who’ve been on prednisone for years, never thought twice about their eyes… until they couldn’t read their grandkids’ names on a birthday card. That’s not just cataracts. That’s a life interrupted by a silent side effect we treat like an afterthought.
It’s not about fear. It’s about stewardship. Your body isn’t a machine with separate compartments. It’s a conversation. And if you’re not listening to your eyes, you’re missing half the dialogue.
Ask for the baseline exam. Ask for the alternatives. Ask for the truth. Even if your doctor doesn’t bring it up, you owe it to yourself to say: ‘What’s this doing to me?’
Because sometimes, the thing that saves your breath is stealing your sight.
Nader Bsyouni
December 24, 2025 AT 21:23Kiranjit Kaur
December 25, 2025 AT 08:04Thank you for this. I’ve been on oral steroids for lupus for 18 months and didn’t realize how much risk I was taking. Just booked my first eye exam in 2 years. Also asked my rheumatologist about loteprednol-she hadn’t mentioned it but said she’ll look into switching me. Small steps, but they matter. 💪👁️
jenny guachamboza
December 27, 2025 AT 04:27Tarun Sharma
December 28, 2025 AT 04:25Thank you for the detailed and clinically accurate information. The emphasis on early monitoring is essential. I would add that ophthalmologists should maintain documentation of steroid exposure in patient records to facilitate longitudinal risk assessment.
Jamison Kissh
December 29, 2025 AT 20:32What struck me most isn’t the science-it’s the silence. We talk about side effects like nausea or weight gain. But eye damage? No one mentions it. No ads. No warning labels on prescriptions. No ‘did you know?’ pop-ups. It’s like the medical system decided some harms are too inconvenient to admit.
And yet, the data is clear. One in three responders. 35% of cases in people with no history. That’s not rare. That’s systemic.
Why aren’t we screening everyone on long-term steroids like we do for cholesterol or blood pressure? Because it’s not profitable? Because it’s not sexy? Or because we still treat vision as a luxury, not a right?
It’s not enough to say ‘get checked.’ We need mandates. We need education. We need doctors to treat the whole body-not just the disease they’re paid to fix.
Candy Cotton
December 30, 2025 AT 04:23As an American citizen who has paid taxes for decades, I find it unacceptable that our healthcare system allows such preventable blindness to occur. In Germany, they have mandatory eye screenings for all steroid users. In Japan, they use AI to monitor intraocular pressure remotely. Here? We rely on patients to ask. That’s not healthcare. That’s negligence. I urge all Americans to demand legislation mandating eye exams with steroid prescriptions. This is not a personal responsibility issue-it’s a national failure.
Gabriella da Silva Mendes
December 31, 2025 AT 11:00I’m so tired of this. I’ve been on prednisone for 5 years for my autoimmune thing. I’ve had 3 eye exams. They said I’m fine. Then I got a new doctor who said ‘oh wow your pressure is 22’ and I was like ‘wait what??’ I just feel like every single doctor is just winging it and I’m the guinea pig. Also I think the FDA is in bed with Big Pharma. Why else would they let these drops be sold without a warning that says ‘may cause blindness’ in giant letters? 🤦♀️👁️🗨️💀
Sam Black
December 31, 2025 AT 12:22This post made me pause. I’ve been using steroid inhalers for asthma for over a decade. I never thought about my eyes. I thought ‘it’s just an inhaler, it’s not going in my eyes.’ But now I wonder-how much gets absorbed? How much lingers? I’m scheduling an exam this week. Thank you for making me see what I didn’t know I was ignoring.
There’s something deeply human about this: we take medicine to live better, but we rarely ask how it changes the way we see the world. Literally.
Cara Hritz
January 1, 2026 AT 10:01Tony Du bled
January 3, 2026 AT 01:27My cousin got cataracts from steroid cream he used for eczema. He didn’t even know it was steroids. Just thought it was ‘that good lotion.’ Took him months to realize his vision was fading. He’s 32. Had surgery. Now he’s got new lenses. But he still gets anxious every time he sees a doctor with a prescription.
It’s not the drug. It’s the lack of context. We’re handed pills and drops like candy. No one says: ‘this might change how you see your child’s face.’
Jim Brown
January 3, 2026 AT 04:01The tragedy lies not in the mechanism of steroid-induced ocular pathology, but in the epistemic asymmetry between medical knowledge and patient awareness. The data is robust, the guidelines are clear, yet the dissemination remains fragmented. This is not a failure of pharmacology-it is a failure of communication architecture within the clinical ecosystem.
Perhaps the solution does not lie in more warnings, but in embedding mandatory ophthalmic risk assessment into the electronic prescribing workflow. A single prompt: ‘Patient on steroids >2 weeks. Recommend baseline IOP measurement.’
That is the kind of systemic intervention that honors both science and humanity.
Julie Chavassieux
January 3, 2026 AT 10:02