Corticosteroid Infection Risk Calculator
Assess Your Infection Risk
Why Corticosteroids Make You More Susceptible to Infections
When you take corticosteroids like prednisone or methylprednisolone for conditions like rheumatoid arthritis, lupus, or asthma, you’re not just calming inflammation-you’re also quietly shutting down parts of your immune system. These drugs mimic cortisol, the body’s natural stress hormone, but at doses far higher than what your body normally produces. That’s where the problem starts. At therapeutic levels, corticosteroids don’t just reduce swelling or pain; they directly interfere with how your body fights off germs.
The biggest issue? Your T cells, the immune system’s frontline soldiers against viruses and intracellular bacteria, get hit hard. Studies show that even moderate doses-like 15 mg of prednisone daily-can cut your T cell count by half within days. These cells don’t just disappear; they’re forced out of circulation, become less active, and eventually die off. Meanwhile, your body’s ability to recognize and destroy invaders like tuberculosis or fungal infections drops dramatically. What’s worse, classic signs of infection-fever, redness, swelling-often don’t show up. One study found that 40% of patients on high-dose steroids had serious infections without a fever. That means you could be getting sicker and not even realize it.
How Much Is Too Much? Dose and Duration Matter
It’s not just about whether you’re on steroids-it’s how much and for how long. The risk of serious infection doesn’t jump suddenly; it climbs steadily. If you’re taking 20 mg or more of prednisone daily for more than 3 to 4 weeks, your infection risk doubles. Every extra 10 mg per day increases that risk by 32%, according to a 2022 analysis of over 100,000 patients. That’s not a small increase-it’s the difference between a manageable risk and a life-threatening one.
Some infections are more common than others. Pneumocystis jirovecii pneumonia (PJP), once rare outside of HIV patients, now accounts for nearly 1 in 5 cases in people on long-term steroids. Tuberculosis can wake up from years of dormancy. Fungal infections like candidiasis and aspergillosis become more likely, especially if you’re in a humid climate or have been in a hospital. And herpes zoster-shingles-hits 3 to 6 times more often in steroid users than in the general population. These aren’t theoretical risks. They happen in real people, often after months of feeling fine.
Preventing Infections: What Actually Works
There’s no magic shield against infection when you’re on steroids-but there are proven steps that cut risk dramatically. The first is prophylaxis. If you’re on 20 mg or more of prednisone daily for over 4 weeks, you should be on trimethoprim-sulfamethoxazole (Bactrim or Septra) to prevent PJP. This single drug reduces PJP cases from over 5% down to less than 0.5%. It’s cheap, simple, and backed by decades of data.
Before starting steroids, especially at 15 mg/day or higher, you need a tuberculosis screen. That means either a skin test or a blood test (IGRA). If you test positive for latent TB, you’ll need a 9-month course of isoniazid or a 4-month course of rifampin. Done right, this cuts reactivation risk by 90%. Skipping this step isn’t just careless-it’s dangerous, especially if you’ve lived in or traveled to areas where TB is common.
Vaccines: What to Get and When
Vaccines are one of your best defenses-but timing matters. Live vaccines like MMR, varicella, or nasal flu spray are off-limits once you start steroids. They can cause the disease they’re meant to prevent. But inactivated vaccines? Those are safe and critical. Get your pneumococcal vaccine (Prevnar 20 or Pneumovax 23), yearly flu shot, and COVID-19 boosters before you start treatment. If you’re already on steroids, get them anyway, but know that your immune system might not respond as well. One study showed only 42% of people on high-dose steroids developed protective antibodies after the flu shot, compared to 78% of healthy people. That doesn’t mean skip it-it means get it early and repeat if needed.
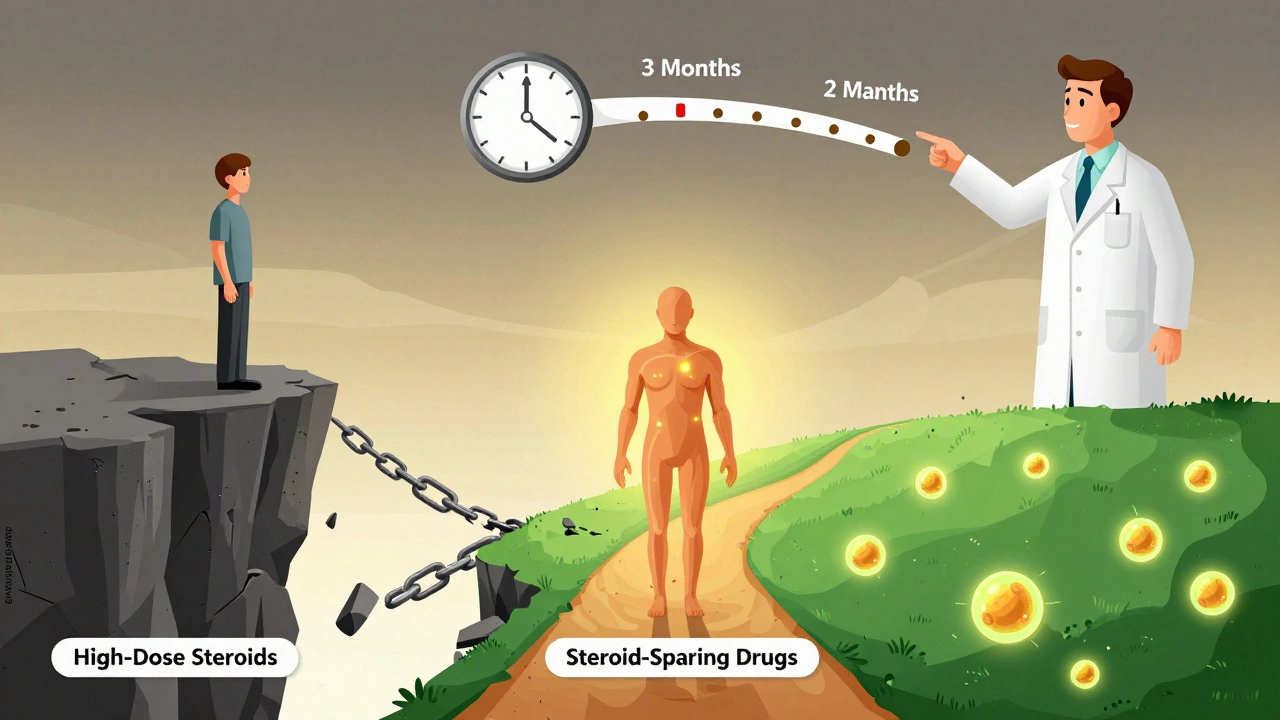
Lower the Dose, Lower the Risk
The most powerful tool you have isn’t a drug or a vaccine-it’s your doctor’s willingness to taper you off. The longer you stay on high-dose steroids, the higher your risk. Experts agree: the lowest effective dose for the shortest time is the golden rule. Rapid tapering-cutting the dose faster than traditional guidelines suggest-can reduce infection rates by 37%. Many patients can switch to steroid-sparing drugs like methotrexate, azathioprine, or biologics within 4 to 8 weeks. One Reddit user shared that after 3 months on prednisone, his rheumatologist switched him to methotrexate. He hasn’t had a flare in 6 months-and hasn’t caught a cold since. That’s not luck. That’s smart management.
Monitoring and Awareness: Don’t Wait for Symptoms
Because steroids mask inflammation, you can’t rely on how you feel. A routine blood test every 2 to 4 weeks can catch lymphopenia (low lymphocyte count), which signals you’re in high-risk territory. An absolute lymphocyte count below 1,000 cells/μL means your immune system is significantly suppressed. In high-risk areas, monthly chest X-rays are recommended to catch early signs of TB or fungal pneumonia. And if you develop a cough, fever, rash, or even just unexplained fatigue, don’t wait. Call your doctor immediately. Don’t assume it’s just a cold. In steroid users, even a minor infection can spiral fast.
Why So Many People Are Still at Risk
Despite clear guidelines, only about half of patients on long-term steroids get the right prevention. The FORWARD registry found that 48% of people never received PJP prophylaxis, even when they met the criteria. Why? Some doctors assume the patient will ask. Others think the risk is low. Many patients don’t know enough to push for it. But the data is clear: if you’re on steroids long-term, you’re at risk-and prevention is simple, safe, and effective. You don’t have to accept infection as part of the deal.
The Future: Safer Steroids on the Horizon
Researchers are working on a new class of drugs called selective glucocorticoid receptor modulators, or SEGRMs. One, called vamorolone, showed the same anti-inflammatory power as prednisone in Duchenne muscular dystrophy-but with 47% fewer infections. It’s not yet widely available, but it’s a sign of where things are headed. In the next 5 years, we may use genetic tests to predict who’s most vulnerable to steroid-induced immunosuppression and tailor prevention exactly to their risk. Until then, the tools we have work. You just need to use them.
What You Can Do Right Now
- If you’re on prednisone or another steroid for more than 3 weeks, ask your doctor: Am I at risk for PJP?
- If you’re on 15 mg/day or more, ask: Have I been screened for TB?
- Have you gotten your pneumococcal, flu, and COVID vaccines? If not, schedule them now.
- Are you on the lowest possible dose? Ask about switching to a steroid-sparing drug.
- Keep track of your lymphocyte count. If it drops below 1,000, your risk goes up.
- Don’t ignore fatigue, cough, or fever-even if you don’t feel sick.
Steroids save lives. But they also come with hidden dangers. The key isn’t avoiding them-it’s using them wisely. With the right precautions, you can control your disease without becoming a target for preventable infections.
Can corticosteroids cause pneumonia?
Yes. Corticosteroids significantly increase the risk of pneumonia, especially a rare but serious type called Pneumocystis jirovecii pneumonia (PJP). This infection typically affects people with weakened immune systems and can be fatal if not caught early. Patients taking 20 mg or more of prednisone daily for more than 4 weeks are at highest risk. Prophylactic antibiotics like trimethoprim-sulfamethoxazole reduce PJP incidence by over 90%.
Is it safe to get vaccines while on steroids?
Inactivated vaccines like flu, pneumococcal, and COVID-19 shots are safe and recommended-even while on steroids. But live vaccines (like MMR, varicella, or nasal flu spray) are dangerous and should be avoided. Ideally, get all necessary vaccines at least 2 weeks before starting steroids. If you’re already on them, get them anyway, but understand your immune response may be weaker. Antibody levels after vaccination can be 30-50% lower than in healthy people.
How long does steroid-induced immunosuppression last?
The effects begin within days of starting treatment and can last for weeks after stopping, depending on the dose and duration. For short courses (under 2 weeks), immune function usually rebounds within a few weeks. For long-term use (over 1 month), it can take 3 to 6 months or longer for lymphocyte counts and immune responses to return to normal. This is why rapid tapering and early use of steroid-sparing drugs are so important.
Can you get tuberculosis from steroids?
No, you don’t get TB from steroids-but steroids can wake up a dormant TB infection. If you’ve been exposed to TB in the past, even decades ago, the drug can suppress your immune system enough for the bacteria to reactivate. That’s why screening with a skin test or blood test is mandatory before starting long-term steroid therapy. Treating latent TB before starting steroids reduces reactivation risk by 90%.
Do all corticosteroids carry the same infection risk?
Yes, when used systemically (oral, IV, or intramuscular), all glucocorticoids-prednisone, methylprednisolone, dexamethasone, hydrocortisone-carry similar immunosuppressive risks. The key factor is the total daily dose converted to prednisone equivalent. Inhaled or topical steroids have much lower systemic absorption and pose minimal infection risk unless used in very high doses over long periods. Always ask your doctor what your daily prednisone equivalent dose is.

Webster Bull
December 12, 2025 AT 16:32John Fred
December 14, 2025 AT 02:01Harriet Wollaston
December 15, 2025 AT 08:38Lauren Scrima
December 16, 2025 AT 05:57Casey Mellish
December 18, 2025 AT 03:59Hamza Laassili
December 18, 2025 AT 18:38Emily Haworth
December 19, 2025 AT 09:35Himmat Singh
December 20, 2025 AT 20:14