Antihistamine Safety Checker for Seniors
First-generation antihistamines like Benadryl can increase fall risk by over 50% in older adults. Check if your antihistamine is safe for seniors.
Every year, nearly one in four older adults falls. For many, the cause isn’t slippery floors or poor lighting-it’s a pill they took for allergies or sleep. First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and brompheniramine are still widely used by seniors, often without knowing the real danger. These drugs don’t just stop sneezing-they slow down the brain, blur vision, and wreck balance. And in older bodies, the effects last longer, hit harder, and can lead to broken hips, hospital stays, or worse.
Why These Medications Are So Dangerous for Seniors
First-generation antihistamines were designed in the 1940s to block histamine and ease allergy symptoms. But unlike newer versions, they easily slip through the blood-brain barrier. Once inside, they act like sedatives, slowing nerve signals that control movement, balance, and reaction time. In a 70-year-old, the half-life of diphenhydramine stretches from 8.5 hours to over 13 hours. That means if someone takes a 25mg tablet at 8 a.m., they’re still feeling drowsy at 8 p.m.-and maybe even at midnight.
These drugs also have strong anticholinergic effects. On the Anticholinergic Cognitive Burden Scale, diphenhydramine scores a 4-meaning it’s one of the most potent. That’s the same level as some antidepressants and bladder medications linked to dementia. A 2018 meta-analysis in Osteoporosis International found that older adults taking these antihistamines had a 54% higher risk of injurious falls and a 43% higher risk of fractures. The CDC’s STEADI program lists them alongside benzodiazepines and opioids as top fall-risk medications.
It’s not just falls. A 2023 study in Neurology Advisor found that seniors on these meds were 2.3 times more likely to develop delirium in the hospital. Delirium means confusion, hallucinations, and agitation-conditions that make falling even more likely. And yet, these drugs are still sold over the counter with labels that barely warn about dizziness or drowsiness.
The Safer Alternatives That Actually Work
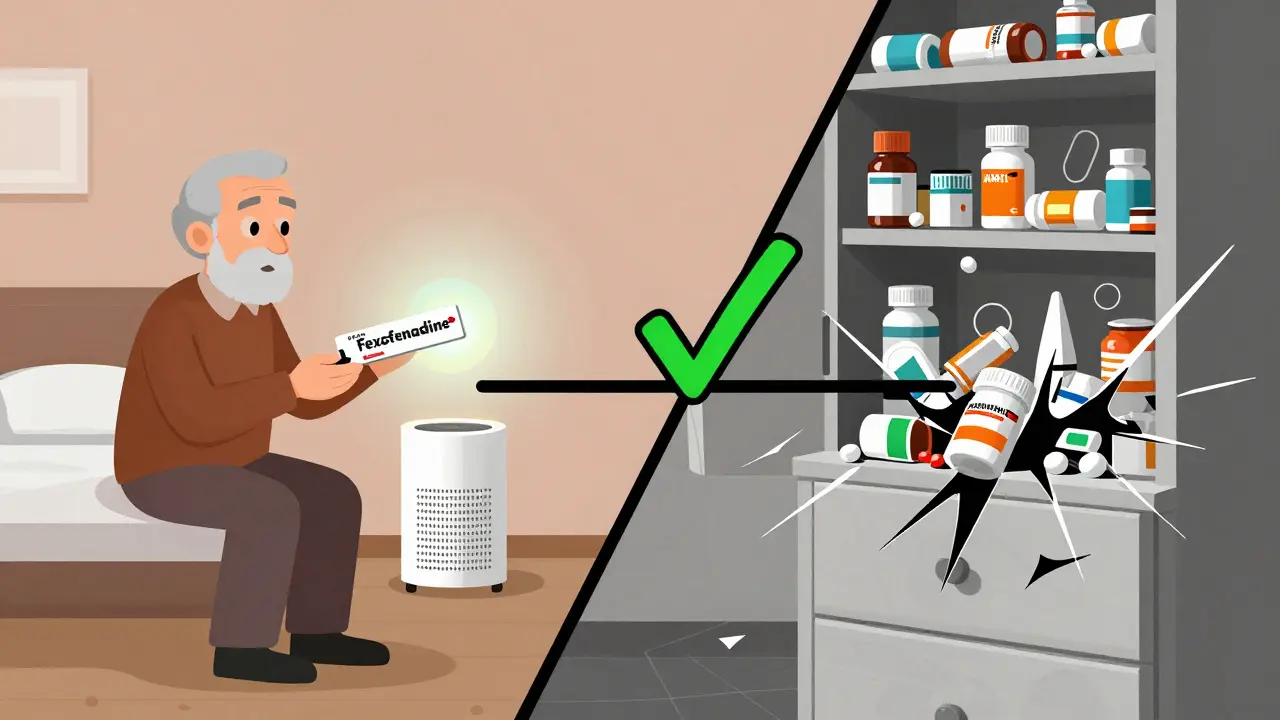
There’s a better way. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were developed specifically to avoid the brain. They don’t cross the blood-brain barrier easily, so they don’t cause the same level of sedation. Studies show they don’t increase fall risk at all.
Here’s the difference in real numbers:
- Diphenhydramine causes drowsiness in 15-20% of users; fexofenadine causes it in only 6%.
- Chlorpheniramine increases fall risk by 87% compared to no use; loratadine shows no increase.
- Fexofenadine has an anticholinergic score of 0. Diphenhydramine? Score of 4.
Even among second-generation options, there’s variation. Cetirizine still causes drowsiness in about 14% of older adults-twice as many as fexofenadine. So if someone needs an antihistamine, fexofenadine is the safest pick. It’s just as effective for allergies, doesn’t impair thinking, and doesn’t make you wobbly on your feet.
The American Geriatric Society’s Beers Criteria has labeled first-generation antihistamines as “potentially inappropriate” for older adults since 2015-and strengthened that warning in 2025. Yet, a 2019 study found doctors still prescribed them at nearly the same rate for seniors as for younger people. Why? Because many don’t know the risks. Or worse, they assume OTC means safe.
What to Do If You or a Loved One Is Taking These Meds
If someone you care about is taking Benadryl for allergies, sleep, or even an upset stomach, here’s what to do:
- Don’t stop cold turkey. Sudden withdrawal from diphenhydramine can cause rebound itching, insomnia, or anxiety. Work with a doctor or pharmacist to taper slowly.
- Switch to fexofenadine. For allergies, it’s just as effective and far safer. The dose is 180mg once daily. No need to split it.
- Check all meds. Many seniors take multiple OTC products. Diphenhydramine hides in sleep aids, cold medicines, and even some pain relievers. Read every label.
- Ask for a brown bag review. Take all pills, vitamins, and supplements to a pharmacist. They’ll spot hidden antihistamines and other fall risks. Studies show this reduces falls by 26%.
For sleep issues, don’t reach for Benadryl. It’s not a sleep aid-it’s a sedative with long-term risks. Instead, try sleep hygiene: no screens after 8 p.m., consistent bedtime, keeping the bedroom cool and dark, and avoiding caffeine after noon. If needed, melatonin (3mg) is a safer, non-anticholinergic option.
Non-Medication Ways to Control Allergies
Antihistamines aren’t the only way to manage allergies. In fact, reducing exposure works better-and has zero side effects.
- Nasal saline irrigation. Using a neti pot or squeeze bottle with sterile salt water reduces allergy symptoms by 35-40%, according to JAMA Otolaryngology.
- Allergen-proof bedding. Dust mites trigger most indoor allergies. Special covers for pillows and mattresses reduce exposure by 83%.
- HEPA air filters. A good one removes 99.97% of airborne allergens-pollen, pet dander, mold spores. Place one in the bedroom.
- Shower before bed. Washing off pollen from hair and skin prevents nighttime symptoms.
These steps don’t just reduce the need for meds-they improve overall quality of life. No drowsiness. No confusion. No fear of falling.

Environmental Fixes That Save Lives
Even if you can’t stop the medication right away, making the home safer helps.
- Install grab bars. In the bathroom, near the toilet and shower. Reduces fall risk by 28%.
- Improve lighting. Add nightlights in hallways and bathrooms. Falls drop by 32% with better light.
- Remove rugs and cords. Tripping hazards are the #1 cause of home falls.
- Wear non-slip shoes. Even socks with rubber dots help. Avoid slippers with smooth soles.
These changes cost little but save lives. A single fall can lead to a broken hip, surgery, long-term care, or death. For every dollar spent on home safety, $3.50 is saved in healthcare costs.
What’s Changing in 2026
The tide is turning. Since 2024, Medicare’s Annual Wellness Visit now requires doctors to review all medications for fall risk-including antihistamines. Pharmacies are starting to flag high-risk prescriptions automatically. The FDA now requires stronger warnings on OTC sleep aids containing diphenhydramine.
And new drugs are coming. Two next-generation antihistamines (AGS-2025-01 and FEX-AGE-101) are in Phase II trials. Early results show 89% less drowsiness than diphenhydramine-with no loss of allergy relief. These could be available by 2028.
But we don’t have to wait. The tools we have now-safer meds, home fixes, pharmacist reviews-are enough to prevent thousands of falls. The question isn’t whether we can do better. It’s whether we will.
Are over-the-counter antihistamines safe for seniors?
No, first-generation OTC antihistamines like diphenhydramine (Benadryl) and chlorpheniramine are not safe for older adults. They increase fall risk, cause confusion, and can lead to delirium. Even though they’re sold without a prescription, they carry serious risks. Safer alternatives like fexofenadine (Allegra) or loratadine (Claritin) are available over the counter and don’t carry the same dangers.
What’s the difference between first and second-generation antihistamines?
First-generation antihistamines (like Benadryl) cross into the brain and cause drowsiness, dizziness, and impaired balance. Second-generation antihistamines (like Claritin, Zyrtec, Allegra) are designed to stay out of the brain, so they treat allergies without sedating you. Studies show first-gen drugs increase fall risk by over 50%, while second-gen show no significant increase.
Can I switch from Benadryl to Allegra on my own?
You can switch from diphenhydramine to fexofenadine without a prescription, but it’s best to do it with guidance. Stopping suddenly can cause rebound symptoms like itching or trouble sleeping. Talk to your pharmacist or doctor first. They can help you taper off safely and recommend the right dose of the new medication.
Why do doctors still prescribe diphenhydramine to seniors?
Many doctors aren’t aware of the updated guidelines, or they assume OTC means safe. Others prescribe it because it’s cheap and familiar. But evidence is clear: it’s outdated and dangerous for older adults. The American Geriatric Society has warned against it for over a decade. Patients should ask for safer options and push back if they’re offered diphenhydramine as a first choice.
How can I check if my meds are risky?
Bring all your pills-prescription, OTC, and supplements-to a pharmacist for a "brown bag review." They’ll scan for anticholinergic drugs, sedatives, and other fall risks. You can also use the CDC’s STEADI checklist online or ask your doctor to run a medication review during your annual wellness visit, which is now required for Medicare patients.

kenneth pillet
January 17, 2026 AT 15:24Been telling my grandma to ditch Benadryl for years. She thought it was just a sleep aid. Turns out she was taking it for allergies too. Switched her to Allegra last month. No more midnight wanderings. She’s actually sleeping better now.
Naomi Keyes
January 18, 2026 AT 15:07Let’s be real-this isn’t about medicine. It’s about corporate greed. The FDA lets these dangerous OTC drugs stay on shelves because Big Pharma makes billions off seniors being confused and falling. And who pays? Medicare. And you. And me. It’s a scam wrapped in a pink pill bottle.
Dayanara Villafuerte
January 20, 2026 AT 05:12My abuela used to take Benadryl for everything 😭 Then she fell in the shower and broke her hip. Now she takes Zyrtec and uses a neti pot. She’s dancing again at family gatherings 🕺💃 #LessDrugsMoreDancing
Robert Cassidy
January 22, 2026 AT 01:26They want you to think this is about safety. It’s not. It’s about control. Who gets to decide what you take? The FDA? Your doctor? The pharmaceutical lobby? We’re not children. Let seniors choose. If they want to sleep with their eyes closed and risk a fall-let them. Freedom means risk.
Andrew Qu
January 23, 2026 AT 03:39As a geriatric pharmacist, I see this daily. A patient comes in on 8 meds. Five of them are anticholinergic. One is diphenhydramine in a nighttime cold med. They say, ‘But it’s OTC!’ I say, ‘So is cyanide if you call it ‘mint flavor.’’ The Beers Criteria isn’t a suggestion-it’s a lifeline. If your doc prescribes Benadryl, ask why. Then ask for a second opinion.
rachel bellet
January 24, 2026 AT 22:54The data is unequivocal: anticholinergic burden > 3 is associated with a 1.5x increase in all-cause mortality in adults over 65, per the 2022 JAMA Internal Medicine meta-analysis. Diphenhydramine’s score of 4 places it in the highest-risk tier-alongside amitriptyline and oxybutynin. Yet, it remains OTC. This is a public health failure of catastrophic proportions. Regulatory inertia is killing people.
Jodi Harding
January 25, 2026 AT 15:05My dad took Benadryl for sleep for 20 years. He didn’t know it was making him foggy. One day he forgot his own name. Not a joke. He was in the ER. Now he uses melatonin. And he remembers my birthday again.
Pat Dean
January 26, 2026 AT 15:20Of course this is true. But why are you only talking about antihistamines? What about the 30 other drugs in their cabinet? The statins that cause muscle loss? The beta-blockers that make them dizzy? This is just the tip of the iceberg. You’re distracting people from the real problem: doctors don’t stop prescribing junk because they’re lazy. And patients don’t ask because they’re too scared to challenge authority.
Jay Clarke
January 27, 2026 AT 20:28People are dying because they’re too polite to ask questions. My aunt took diphenhydramine for ‘a little help sleeping’-until she started hallucinating and tried to jump out the window. We found it in her nightstand next to her crossword puzzle. No one told her it was dangerous. No one asked. That’s not negligence. That’s betrayal.
Selina Warren
January 29, 2026 AT 17:14Imagine if we treated kids this way. Give them a sedative for a runny nose and call it ‘safe’? We’d be in court. But seniors? They’re invisible. Their bodies are seen as ‘past their prime.’ So we give them dangerous drugs and call it compassion. It’s not compassion. It’s abandonment dressed in a white coat.
christian Espinola
January 31, 2026 AT 15:37There’s a reason these drugs are still sold. The FDA is corrupt. The same people who approved OxyContin approved diphenhydramine. They’re all part of the same network. You think this is about safety? It’s about profit. And the media won’t cover it because they’re owned by the same corporations. Wake up.
Stacey Marsengill
February 1, 2026 AT 23:13I used to think Benadryl was harmless. Then I watched my mom turn into a zombie after one pill. She didn’t recognize me for three days. The worst part? She still swears it’s ‘the only thing that works.’ I’ve cried so many times over this. Not because she’s sick. But because no one told her.
Robert Davis
February 3, 2026 AT 03:02Everyone’s so focused on the meds. But what about the real issue? Seniors are lonely. They take these pills because they’re bored. Or scared. Or just want to feel something. You can’t just swap a drug for another drug. You need to give them purpose. A garden. A grandkid. A reason to wake up. Then they won’t need the pill.
Chuck Dickson
February 4, 2026 AT 14:09Listen-I’m not a doctor. But I’m a son. My dad’s 78. He used to take Benadryl for sleep. I sat him down. Showed him the numbers. We switched to Allegra. He’s walking the dog every morning now. No more tripping over the rug. No more confusion at breakfast. He says he feels like himself again. It’s not magic. It’s just… better choices. You can do this. Start today.
Andrew Qu
February 5, 2026 AT 02:24One thing I didn’t see mentioned: the cost difference. Fexofenadine is $4 at Walmart. Benadryl is $3. So price isn’t a barrier. It’s ignorance. And that’s the real enemy. Pharmacies should have a sticker on every diphenhydramine bottle: ‘WARNING: This drug increases your risk of falling by 54%. You are 2.3x more likely to end up in the hospital.’ Simple. Clear. Mandatory.