Before 1984, if you needed a generic version of a prescription drug, you were out of luck. The system wasn’t broken-it was practically nonexistent. Generic drugs weren’t banned, but the rules made them nearly impossible to bring to market. Companies had to run full clinical trials to prove their version was safe and effective, even though the brand-name drug had already been approved. That meant years of extra time and millions of dollars in costs. For most generic manufacturers, it just wasn’t worth it. As a result, fewer than 1 in 5 prescriptions filled in the U.S. in 1983 were for generics. The rest? Brand-name drugs, often at full price.
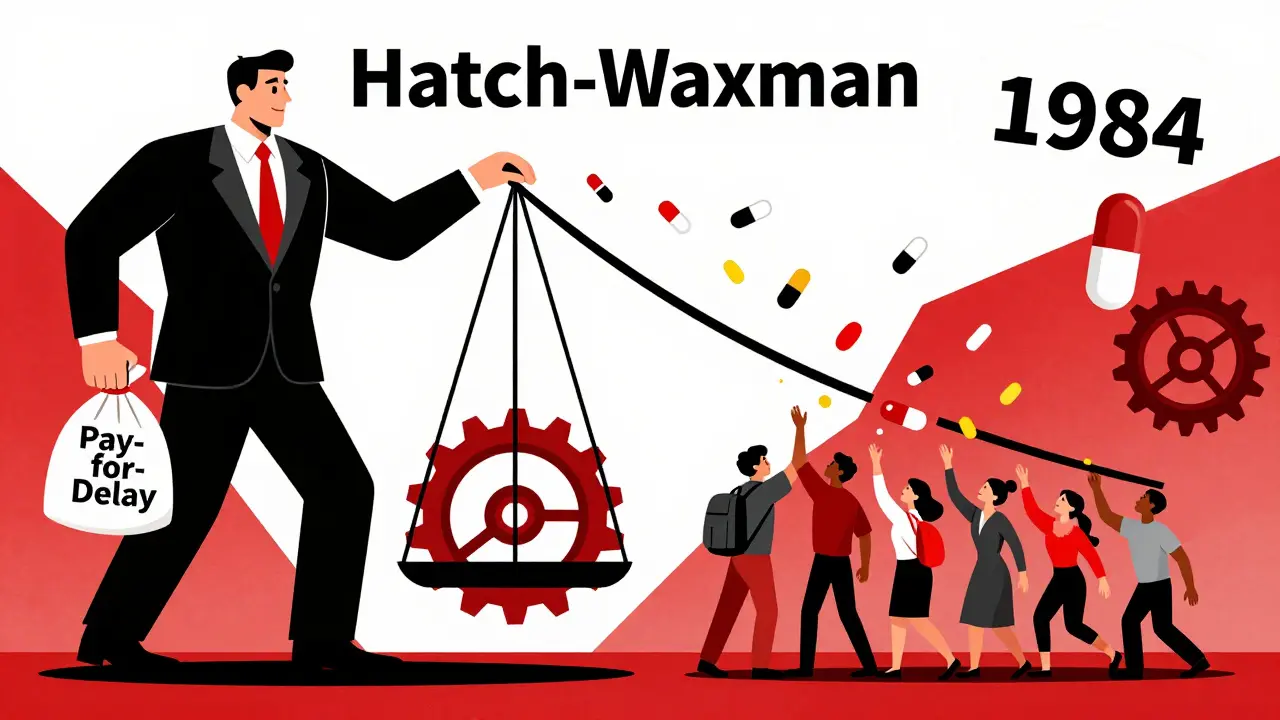
What the Hatch-Waxman Act Actually Did
The Drug Price Competition and Patent Term Restoration Act of 1984-better known as the Hatch-Waxman Amendments-changed all of that. It didn’t just tweak the system. It rebuilt it from the ground up. Named after its two sponsors, Senator Orrin Hatch and Representative Henry Waxman, the law created a clear path for generic drugs to enter the market without reinventing the wheel.
At its core, Hatch-Waxman introduced the Abbreviated New Drug Application (ANDA). This allowed generic manufacturers to skip expensive clinical trials. Instead, they only had to prove their drug was bioequivalent to the brand-name version. That means it delivered the same amount of active ingredient into the bloodstream at the same rate. No need to prove safety again. No need to repeat efficacy studies. Just show the body reacts the same way.
This single change slashed development costs by 80-90%. Suddenly, making a generic version of a drug wasn’t a financial gamble-it was a smart business move. And that’s exactly what happened.
The Patent Game: How Brand-Name Companies Got Their Due
But if you’re a company that spent $1 billion and 10 years developing a new drug, you don’t want generic competitors showing up the day your patent expires. Hatch-Waxman knew that. So it gave brand-name manufacturers something they desperately wanted: patent term restoration.
When the FDA reviews a new drug, it takes time. On average, two to five years of a drug’s 20-year patent life were eaten up by the approval process. Hatch-Waxman allowed companies to extend their patent by up to five years to make up for that lost time. That meant more years of market exclusivity, more revenue to fund future research.
The law also created new types of exclusivity. A new chemical entity got five years of protection. A new use for an existing drug? Three years. Orphan drugs? Seven years. These weren’t patents-they were regulatory shields, giving companies breathing room before generics could even apply.
The Safe Harbor: Letting Generics Start Early
Here’s where things got clever. Before Hatch-Waxman, a 1984 court case (Roche v. Bolar) ruled that even testing a generic version before a patent expired was illegal patent infringement. That meant generic companies had to wait until the patent expired to even start development. By then, they were already behind.
Hatch-Waxman fixed that with a simple but powerful rule: activities done solely to gather data for FDA approval are exempt from patent infringement. This is now called the “safe harbor” provision under 35 U.S.C. § 271(e)(1). It lets generic companies begin bioequivalence studies, manufacturing, and even packaging while the brand-name drug’s patent is still active.
This single change turned the generic industry from a passive observer into an active competitor. Companies could now plan years ahead. They could time their applications to hit the market the moment the patent ran out.
The 180-Day Prize: Why the First Generic Company Wins Big
One of the most powerful incentives in Hatch-Waxman is the 180-day exclusivity period for the first generic company to file an ANDA with a Paragraph IV certification.
What’s a Paragraph IV certification? It’s when a generic company says, “Your patent is invalid, or we don’t infringe it.” That’s a direct challenge. And if the brand-name company sues, the FDA can’t approve the generic for 30 months-unless the court rules in the generic’s favor sooner.
But if the first filer wins, they get 180 days of exclusive market access. No other generics can enter. That’s a massive advantage. During those six months, the first generic can charge significantly more than later entrants-sometimes even close to brand-name prices-while still making huge profits.
This rule was meant to encourage patent challenges. And it worked. But it also created a loophole. Some companies started filing Paragraph IV certifications just to block others. Others teamed up with brand-name firms in “pay-for-delay” deals: the brand pays the generic to hold off on launching. The Federal Trade Commission found 668 such deals between 1999 and 2012, costing consumers an estimated $35 billion a year.
The Results: 90% of Prescriptions, 85% Less Cost
The numbers don’t lie. In 1983, generics made up less than 19% of prescriptions. In 2023, they made up nearly 90%. Today, over 10,000 generic drugs are available in the U.S. They cost, on average, 80-85% less than their brand-name equivalents.
That’s not just savings. That’s access. Millions of Americans who couldn’t afford insulin, blood pressure meds, or antidepressants before 1984 can now take them because of Hatch-Waxman. It didn’t just lower prices-it saved lives.
Where the System Is Straining
But the balance Hatch and Waxman struck in 1984 is under pressure.
Brand-name companies now use tactics the law never intended. “Evergreening” is one: making tiny changes to a drug-like switching from a pill to a liquid-to get a new patent and reset the clock. “Citizen petitions” are another: filing baseless complaints with the FDA to delay generic approvals. And “pay-for-delay” deals still happen, even though they’re now illegal in many cases.
The FDA has responded. The Generic Drug User Fee Amendments (GDUFA), introduced in 2012 and renewed in 2017 and 2022, gave the agency more money to hire reviewers. The average ANDA review time dropped from 30 months in 2012 to under 12 months by 2022. That’s progress.
But the 180-day exclusivity rule remains messy. When two companies file on the same day, the FDA now splits the exclusivity. Still, companies spend millions on legal teams just to be the first to file. It’s a race that often has more to do with lawyers than science.
Is Hatch-Waxman Still Working?
Yes-and no.
It delivered on its core promises: generics are now the backbone of U.S. pharmacy. Billions in savings. Widespread access. Innovation still happens-new drugs keep getting approved. The system works.
But the compromises it made are being exploited. The law assumed good faith. It didn’t predict sophisticated legal gamesmanship. Today, the biggest barrier to affordable drugs isn’t the FDA-it’s the playbook of brand-name companies using the law’s own rules against it.
Legislators are trying. The 2023 Preserve Access to Affordable Generics and Biosimilars Act aims to crack down on pay-for-delay deals. But without fixing the incentives, the problem will keep coming back.
Hatch-Waxman didn’t just change drug policy. It changed how Americans live. It made medicine affordable. But it also created a battlefield where money and law collide. The question now isn’t whether the law was good-it’s whether we still believe in its original promise: that innovation and access can coexist. Because right now, they’re not.
What is the Hatch-Waxman Act?
The Hatch-Waxman Act, officially the Drug Price Competition and Patent Term Restoration Act of 1984, is U.S. law that created the modern system for approving generic drugs. It lets generic companies skip costly clinical trials by proving bioequivalence to brand-name drugs, while giving brand-name makers extra patent time to make up for FDA review delays.
How did generic drugs work before Hatch-Waxman?
Before 1984, generic manufacturers had to submit full New Drug Applications (NDAs), including their own clinical trials to prove safety and effectiveness-even though the brand-name drug had already been approved. This made generic development too expensive and slow, so very few were available. Less than 19% of prescriptions were for generics in 1983.
What is an ANDA?
ANDA stands for Abbreviated New Drug Application. It’s the streamlined pathway created by Hatch-Waxman for generic drugs. Instead of running new clinical trials, manufacturers prove their product is bioequivalent to the brand-name drug. This cuts development costs by 80-90% and speeds up approval.
Why do generic drugs cost so much less?
Generic drugs cost 80-85% less because they don’t repeat expensive clinical trials. The brand-name company already paid for safety and efficacy studies. Generics only need to prove they deliver the same active ingredient at the same rate. That saves millions in development costs, which translates to lower prices for consumers.
What’s the 180-day exclusivity period?
The first generic company to file an ANDA with a Paragraph IV certification (challenging a patent) gets 180 days of exclusive market access. No other generics can enter during that time. This creates a powerful incentive to challenge weak patents-but it’s also been exploited through strategic filings and pay-for-delay deals.
Is Hatch-Waxman still effective today?
Yes, in terms of access: 90% of U.S. prescriptions are now for generics. But the system is strained. Brand-name companies use legal loopholes like evergreening, citizen petitions, and pay-for-delay deals to delay competition. While the law still works, its original balance between innovation and access is increasingly tilted.
Vince Nairn
January 8, 2026 AT 06:17Adam Gainski
January 9, 2026 AT 13:58Elen Pihlap
January 10, 2026 AT 23:21Sai Ganesh
January 12, 2026 AT 03:57Katrina Morris
January 12, 2026 AT 14:20Andrew N
January 13, 2026 AT 03:26Aparna karwande
January 13, 2026 AT 16:30Jessie Ann Lambrecht
January 14, 2026 AT 19:16Mina Murray
January 16, 2026 AT 12:18Rachel Steward
January 18, 2026 AT 12:12Christine Joy Chicano
January 19, 2026 AT 05:02Anastasia Novak
January 20, 2026 AT 10:12Paul Mason
January 21, 2026 AT 09:10steve rumsford
January 22, 2026 AT 18:17