HIV Medication & Birth Control Interaction Checker
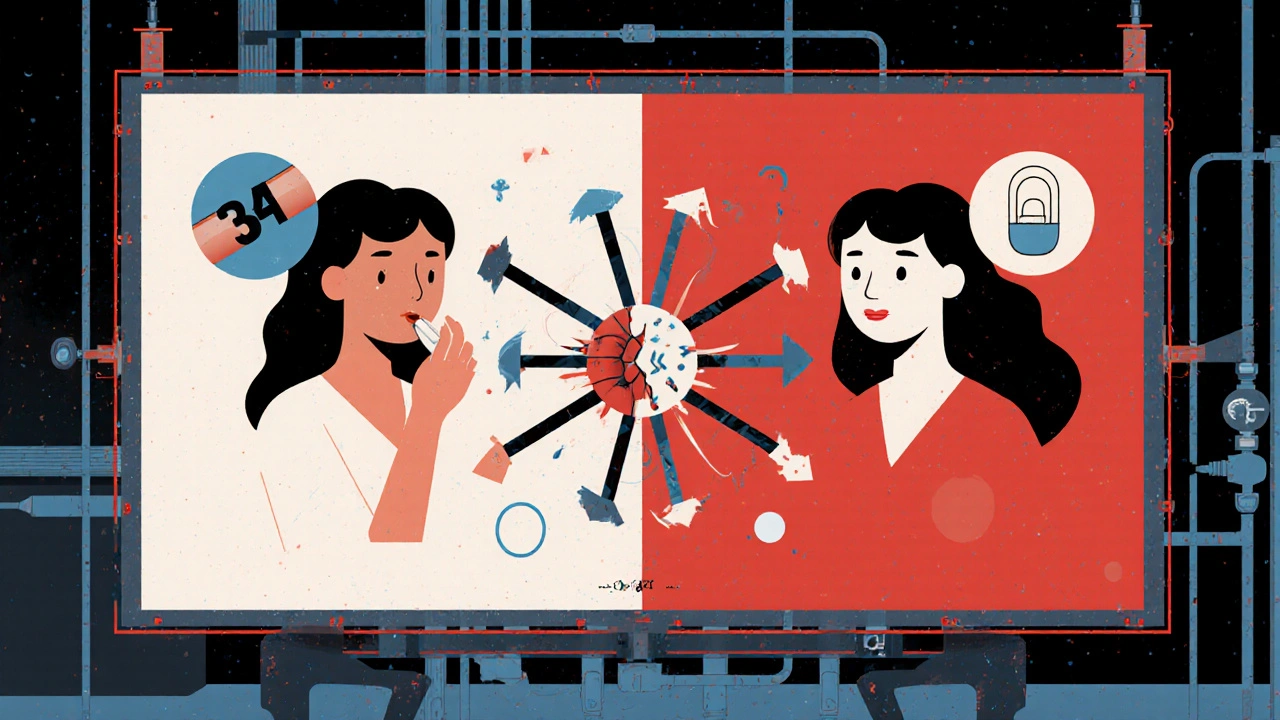
Check Your Contraceptive Safety
This tool helps you determine if your HIV medication interacts with your birth control method. Based on clinical evidence, we'll show you the risk level and recommend the safest options for your situation.
When you're living with HIV and taking antiretroviral drugs, your birth control might not be working the way you think it is. This isn't a myth, a rumor, or something you might have heard on the internet. It's a documented, clinically significant interaction that has led to unintended pregnancies - even in women who take every pill on time, use their patch correctly, and follow every instruction from their doctor.
At the heart of this issue are HIV protease inhibitors, a class of drugs used to block the virus from replicating. These include medications like lopinavir, atazanavir, darunavir, and ritonavir - often given in boosted combinations like lopinavir/ritonavir or darunavir/cobicistat. They’re powerful, life-saving drugs. But they also interfere with how your body processes hormones in birth control.
How Protease Inhibitors Break Down Birth Control
Your body uses enzymes - mainly CYP3A4 - to break down hormones like estrogen and progestin. Birth control pills, patches, rings, and implants all rely on these hormones staying at steady levels to prevent ovulation. But HIV protease inhibitors, especially those boosted with ritonavir, mess with that system. They either slow down or speed up how fast your body clears these hormones.
Take the contraceptive patch, for example. A 2010 study found that when women used it with lopinavir/ritonavir, their estrogen levels dropped by 45%. That’s not a small dip - it’s enough to leave them unprotected. In another study, women using the vaginal ring (NuvaRing) with efavirenz had subtherapeutic hormone levels in 38% of cases. That means the ring wasn’t delivering enough hormone to stop ovulation, even though it was in place.
And it’s not just about pills. Even long-acting methods like implants can be affected. The International AIDS Society-USA warned in 2019 that etonogestrel implants (like Nexplanon) can lose up to 60% of their hormone levels when used with ritonavir-boosted regimens. That’s not just a risk - it’s a failure waiting to happen.
What Birth Control Methods Are Risky?
Not all birth control is equally affected. Here’s what the data shows:
- Combined oral contraceptives (COCs): High risk with efavirenz and ritonavir-boosted PIs. Pregnancy rates jump from the usual 7-8% to 11-15% in women on efavirenz.
- Progestin-only pills (POPs): The WHO classifies these as Category 3 when used with ritonavir-boosted PIs - meaning the risks outweigh the benefits. These pills are especially vulnerable because they contain low hormone doses to begin with.
- Contraceptive patch and ring: Both show significant drops in hormone levels. The ring is particularly problematic due to inconsistent absorption.
- Depo-Provera (DMPA): This injection is generally safer. Studies show mixed results, but most women on DMPA remain protected even with antiretrovirals. WHO still lists it as Category 1 (no restrictions) unless it’s paired with efavirenz, where pregnancy rates climb to 12.3 per 100 woman-years.
- Implants (Nexplanon): Risky with ritonavir-boosted drugs. Not recommended unless no other options exist.
Meanwhile, two methods stand out as safe, reliable, and unaffected:
- Copper IUD: No hormones. No interaction. 99% effective. Works for up to 12 years.
- Hormonal IUD (Mirena, Kyleena, etc.): Releases progestin locally. Minimal systemic absorption. No meaningful interaction with any antiretroviral drug.
These are the gold standard for women on HIV treatment. They don’t rely on daily adherence. They don’t depend on enzyme activity. They just work.

Why Do Doctors Still Miss This?
It’s not that providers are negligent. It’s that the information is scattered, outdated, and often not integrated into routine care.
A 2018 report from the AIDS Clinical Trials Group found that 41% of women received no counseling about contraceptive interactions when they were first diagnosed with HIV. Community clinics were even worse - only 34% had formal protocols compared to 79% at academic centers. Many providers still think, “If she’s taking her pills, she’s protected.” But that’s not true.
Real stories prove it. On HIV forums, women share how they got pregnant despite perfect adherence. One woman on Reddit used Depo-Provera with atazanavir/ritonavir and didn’t realize she was pregnant until 18 weeks. Another woman on HIV.gov took Tri-Sprintec with darunavir/cobicistat and became pregnant. Both had been told their birth control was “fine.”
Dr. Irene Bassett from Massachusetts General Hospital has documented 17 cases of contraceptive failure in just a decade - all in women on lopinavir/ritonavir with oral contraceptives. These aren’t rare outliers. They’re predictable outcomes of known science.
What Should You Do If You’re on HIV Medication?
If you’re taking HIV protease inhibitors - especially those boosted with ritonavir or cobicistat - here’s what you need to do now:
- Check your exact drug regimen. Is it lopinavir/ritonavir? Atazanavir/ritonavir? Darunavir/cobicistat? These are the highest-risk combinations.
- Identify your birth control method. Are you on pills, patch, ring, implant, or injection? Write it down.
- Use the CDC’s interactive tool. The CDC has a free, publicly available drug interaction checker with 147 specific combinations. Type in your HIV meds and your birth control - it tells you the risk level instantly.
- Ask for an IUD or implant. If you’re on a protease inhibitor, the safest, most effective option is a copper or hormonal IUD. Implants are risky unless you’re on dolutegravir or another non-PI drug.
- Don’t rely on condoms alone. They’re important for STI prevention, but not reliable as your only birth control method.
And if you’re thinking about switching your HIV meds? Dolutegravir - an integrase inhibitor - has minimal interaction with hormonal contraceptives. It’s now the first-line treatment for most new patients. If you’re on an older PI-based regimen and want to have children or avoid pregnancy, ask your doctor if switching is an option.
The Bigger Picture: Access and Equity
This isn’t just a medical issue - it’s a justice issue.
In high-income countries, 68% of HIV-positive women use long-acting reversible contraceptives (LARCs) like IUDs and implants. In low-income countries, that number drops to 22%. Why? Because clinics in sub-Saharan Africa often don’t have the tools or training to insert IUDs. A 2022 WHO survey found 63% of clinics there lack immediate IUD insertion capacity.
Women in these settings are forced to choose between effective HIV treatment and effective birth control - and too often, they lose. The result? Unintended pregnancies, unsafe abortions, and maternal health risks.
Programs like FHI360’s color-coded interaction charts have cut contraceptive failures by 37% in 12 African countries. Simple tools - placed at the point of care - make a huge difference. But they’re not everywhere.
What’s Changing? What’s Next?
There’s progress. The WHO is updating its guidelines to reflect newer data. The 2023 draft guidelines propose moving etonogestrel implants from Category 2 to Category 1 when used with dolutegravir - because studies now show only a 12% drop in hormone levels, which isn’t clinically significant.
The NIH-funded NEXT-Study, running across 15 countries, is testing whether levonorgestrel IUDs are safe with 12 different antiretroviral regimens. Results are due by the end of 2025.
And by 2030, experts predict 95% of contraceptive counseling for HIV-positive women will happen in integrated clinics - where HIV care and reproductive health are offered together. Right now, only 47% do. That gap is closing.
But until then, the message is clear: if you’re on HIV protease inhibitors, your birth control might be failing. And you deserve better than guesswork.
Can I still use birth control pills if I’m on HIV protease inhibitors?
It’s not recommended. Combined oral contraceptives (COCs) and progestin-only pills (POPs) are significantly affected by ritonavir-boosted protease inhibitors like lopinavir/ritonavir and darunavir/cobicistat. Studies show hormone levels drop by 30-80%, making pregnancy likely even with perfect use. Avoid these methods unless no other options are available - and even then, use a backup method like condoms.
Is the birth control implant safe with HIV meds?
Not if you’re on ritonavir-boosted protease inhibitors. Studies show hormone levels from implants like Nexplanon can drop by 40-60%, leaving you unprotected. The International AIDS Society-USA advises against using implants with these drugs. If you’re on dolutegravir or another integrase inhibitor, the risk is much lower - but still check with your provider before choosing this method.
What’s the safest birth control method if I have HIV?
The safest options are the copper IUD and hormonal IUD (like Mirena or Kyleena). Both are 99% effective, don’t rely on hormones circulating in your blood, and aren’t affected by any antiretroviral drugs. They last 5-12 years and require no daily action. If you’re not ready for an IUD, the Depo-Provera shot is usually safe - unless you’re on efavirenz.
Does dolutegravir interfere with birth control?
No, dolutegravir - a common integrase inhibitor - has minimal interaction with hormonal contraceptives. Studies show only small, clinically insignificant changes in hormone levels. It’s now the preferred first-line HIV treatment for women of reproductive age because it doesn’t compromise birth control. If you’re on an older protease inhibitor regimen, ask your doctor if switching to dolutegravir is right for you.
I got pregnant while on HIV meds and birth control. Was it my fault?
No. This is not your fault. These interactions are well-documented, but many providers still don’t discuss them. Over 28% of HIV-positive women surveyed in 2021 reported contraceptive failure while on antiretrovirals, and 63% of those cases involved protease inhibitors. The problem lies in the system - not in your adherence or choices. Talk to your provider about switching to an IUD or implant, and ask for better counseling next time.
If you’re on HIV treatment and want to prevent pregnancy - or if you’re trying to get pregnant - you deserve clear, accurate, and personalized advice. Don’t let outdated assumptions put your health at risk. Ask for the CDC’s interaction checker. Ask for an IUD. Ask for a second opinion. Your body, your choice, your right to safe care.
Andy Feltus
November 20, 2025 AT 00:19So let me get this straight - we’ve got life-saving HIV meds that accidentally turn birth control into a fancy placebo? And the solution is just... an IUD? Like, the same thing we’ve had since the 80s? We’re not talking about a new app or a magic pill. We’re talking about a piece of plastic that costs less than your monthly Netflix subscription and works better than half the stuff Big Pharma sells us. And yet, women are still getting pregnant because their doctor didn’t read the footnote. Classic.
It’s not that people are dumb. It’s that the system is designed to ignore the people it’s supposed to protect. And now we’re surprised when the system fails?
Also, props to the author for not saying ‘just use condoms.’ Condoms are great for STIs. Not great for birth control. And pretending otherwise is just lazy.
Richard Risemberg
November 21, 2025 AT 18:31Y’ALL. I just read this and I’m literally vibrating. This is the kind of info that should be plastered on every clinic wall, shoved into every HIV packet, and screamed from the rooftops like a fire alarm at 3 a.m. We’re talking about women who are already managing a chronic illness, taking meds at the same time every day, fighting stigma - and then on top of that, their birth control is secretly sabotaged by their own meds?!
It’s not just about pregnancy. It’s about autonomy. It’s about being told you’re ‘doing everything right’ while your body is being quietly undermined. And the fact that this isn’t standard counseling? That’s medical malpractice dressed up as ‘overlooked detail.’
Let’s get IUDs in every clinic. Let’s train every provider. Let’s make this a non-negotiable part of HIV care. No more ‘maybe,’ no more ‘probably.’ Just: ‘Here’s your IUD. You’re safe.’
Andrew Montandon
November 22, 2025 AT 12:58Okay, I’m a nurse, and I’ve seen this happen - multiple times. A woman comes in for her HIV follow-up, on lopinavir/ritonavir, on the pill, says she’s ‘never missed a dose.’ Then she shows up pregnant. We all assume she slipped up. But no. The science is crystal clear: the drug kills the hormone levels. Period.
And here’s the kicker - we don’t even ask. Why? Because we’re rushed. Because we assume ‘birth control’ = ‘safe.’ Because we’re not trained on drug interactions beyond the basics.
But it’s not just about pills. The patch? The ring? The implant? All risky. The copper IUD? Perfect. Hormonal IUD? Perfect. Depo? Mostly safe unless you’re on efavirenz.
Bottom line: If you’re on a boosted PI, your birth control is broken. Stop trusting the pill. Go get an IUD. Today. Your future self will thank you.
And yes, CDC’s tool is free. Use it. I’ve printed it and taped it to my desk.
Chuck Coffer
November 22, 2025 AT 14:47Wow. So the solution to a medical problem is... not to fix the meds, not to develop better contraceptives, but to just shove an IUD in every woman and call it a day? How convenient.
What about women who don’t want IUDs? What about those who’ve had bad experiences? What about cultural preferences? What about the fact that IUD insertion requires a specialist - and not every clinic has one?
It’s easy to say ‘just use the copper IUD’ when you’ve never had to sit in a waiting room for six months because your clinic doesn’t have the equipment. This isn’t a tech fix. It’s a systemic failure - and you’re blaming the patient for not choosing the ‘right’ option.
Also, ‘don’t rely on condoms’? Really? That’s your advice? What’s next - ‘just stop having sex’?
Marjorie Antoniou
November 23, 2025 AT 01:41I’m a woman living with HIV, and I got pregnant while on darunavir/cobicistat and the pill. I was terrified. I thought I’d failed. I felt guilty. I cried for days.
Then I found this post. And I realized - it wasn’t me. It was the system. No one told me. Not my doctor, not my pharmacist, not even the pamphlets. I was told ‘take your pill, you’re fine.’
Now I have a hormonal IUD. It’s been two years. I feel free. I don’t think about it. I don’t stress. I just live.
If you’re reading this and you’re on a protease inhibitor - please, please, please talk to your provider. Ask for the CDC tool. Ask for an IUD. You don’t have to accept this. You deserve better.
Frank Dahlmeyer
November 23, 2025 AT 04:17Let’s zoom out for a second - this isn’t just about HIV and birth control. This is about how medicine treats women’s bodies as secondary. We prioritize the virus over the person. We focus on suppression, not sovereignty. We fix the CD4 count but ignore the uterus.
And it’s not just HIV. Think about all the other meds - antidepressants, anticonvulsants, even some antibiotics - that interfere with hormonal contraception. Why is this only getting attention now? Because women are finally speaking up? Because we’re tired of being collateral damage?
There’s a pattern here: when a drug interacts with birth control, the burden falls on the woman to figure it out. Not the manufacturer. Not the provider. Not the FDA. The woman. Always the woman.
So yes, IUDs are great. But what we really need is a world where every drug interaction is flagged in bold, in plain language, in every prescription, every label, every patient portal. No more footnotes. No more assumptions. Just clarity. Because women’s bodies are not experimental variables.
And if you’re a provider reading this - your job isn’t just to treat HIV. It’s to protect reproductive autonomy. Do better.
harenee hanapi
November 24, 2025 AT 00:42OMG I can’t believe this is real. I’ve been on atazanavir/ritonavir for 5 years and I’ve been on the patch the whole time. I had two kids already, but I thought I was protected. I just found out I’m pregnant again and I’m so scared. What if something’s wrong with the baby? What if my meds hurt it? I feel like I’m going to lose my mind. Why didn’t anyone tell me?!
I’m so mad. I trusted my doctor. I followed every rule. And now I’m terrified. I don’t know what to do. Can I still take my meds? Will the baby be okay? Please help. I’m so alone.
Nick Lesieur
November 25, 2025 AT 15:23So… you’re telling me that after 20 years of HIV meds, the only thing that actually works for birth control is a 50-year-old device that requires a doctor to shove it up your ass? Cool. Cool cool cool. I’m sure that’s a *huge* upgrade from the pill.
Also, ‘don’t rely on condoms’? Bro. Condoms are the only thing that protects against STIs AND pregnancy. You’re telling me to ditch the only thing that does both? And replace it with a metal thing that costs $1000 and takes 3 appointments to get? Sounds like a scam.
Also, I’ve seen people get IUDs. It’s not ‘just a quick insert.’ It’s screaming, crying, bleeding for a week. And if you’re trans or nonbinary? Good luck finding a provider who won’t stare at you like you’re a zoo animal.
This isn’t a solution. It’s a band-aid on a broken system. And now we’re pretending it’s the answer.
Angela Gutschwager
November 27, 2025 AT 12:28Got pregnant on the ring + darunavir. No one warned me. Now I have a Mirena. Best decision ever. 😊
Dion Hetemi
November 29, 2025 AT 02:14Let’s be real - this isn’t about science. It’s about money.
Big Pharma doesn’t want you to use an IUD. Why? Because they don’t make money off it. IUDs last 10 years. One-time cost. No refills. No monthly pills. No patches. No rings. No revenue stream.
Meanwhile, they’re selling you $100/month pills that interact with your meds - and then they’re selling you the next-gen version that ‘might’ work better. Meanwhile, the copper IUD? Costs $50. Lasts 12 years. No interaction. No fuss.
So who’s pushing this? Who’s funding the guidelines? Who’s training the doctors? Hint: it’s not the people who profit from IUDs.
Don’t be fooled. This isn’t a medical issue. It’s a capitalist one.
Brian Rono
November 29, 2025 AT 10:14Actually - you’re all wrong. The real issue here is that women are being given *too much* control. Why are we letting them choose birth control at all? Why not just mandate IUDs for all HIV-positive women? That way, we eliminate the ‘risk’ of pregnancy entirely.
And let’s be honest - if you’re on antiretrovirals, you’re already a ‘high-risk’ patient. So why not treat your reproductive system the same way? No more ‘choices.’ No more ‘counseling.’ Just insert. Done.
Also, the fact that you’re even discussing condoms as an option is absurd. Condoms are unreliable. You’re not protecting anyone with them. Just stop pretending.
And if you’re upset about this? Maybe you shouldn’t be sexually active. Simple as that.
seamus moginie
November 30, 2025 AT 13:41Excellent post. Truly. The data is robust, the recommendations are clear, and the tone is appropriately urgent. However, I must point out that the WHO’s Category 1 designation for Depo-Provera with non-efavirenz regimens is not universally accepted - particularly in regions where adherence to injection schedules is inconsistent. The efficacy drops precipitously when injections are delayed beyond 14 weeks, which occurs in up to 30% of cases in rural settings.
Therefore, while IUDs remain the gold standard, the argument for Depo-Provera as a ‘safe’ alternative must be qualified by access to consistent healthcare infrastructure. In the absence of that, even ‘safe’ methods become unreliable.
Thank you for highlighting the equity gap. This is not merely a clinical issue - it is a moral imperative.
Dana Dolan
December 2, 2025 AT 10:32My doctor just switched me from lopinavir/ritonavir to dolutegravir last month. I was so scared to change my meds. But now? I can finally use the patch again without feeling like I’m playing Russian roulette.
Also, I got the Mirena inserted last week. It’s weird, but not painful. And I feel… free. Like I can breathe again.
Thank you for writing this. I’m sharing it with everyone I know.
Andy Feltus
December 3, 2025 AT 20:15Thanks for sharing your story. That’s exactly why we need to push for switching to integrase inhibitors - not just for birth control, but for long-term kidney, bone, and metabolic health too. Dolutegravir isn’t just safer for contraception. It’s safer for your whole body.
And if your provider says ‘it’s too soon to switch’ - ask for the data. The guidelines changed in 2021. You deserve the best care, not the oldest regimen.