Calcium and Blood Pressure Calculator
Estimated Results
Ever wondered why a simple mineral could have a say in your blood pressure? calcium deficiency and hypertension are more intertwined than most people realize. Understanding this link can help you tweak your diet, avoid hidden traps, and keep your heart in good shape.
Key Takeaways
- Low calcium intake can raise blood pressure by affecting hormone balance and vascular tone.
- Clinical studies show a modest but consistent reduction in systolic pressure when calcium intake reaches 1,200mg per day.
- Combining calcium‑rich foods with a low‑sodium, potassium‑rich diet (like the DASH plan) gives the best results.
- Supplements work for some, but excess calcium may increase kidney stone risk, so monitor intake.
- Regular blood‑pressure checks and a balanced diet are the simplest ways to protect your heart.
What Is Calcium Deficiency?
Calcium deficiency is a condition where the body does not receive enough calcium to meet its physiological needs. Calcium is the most abundant mineral in the human body, crucial for bone strength, muscle contraction, nerve signaling, and blood clotting. When intake falls below the Recommended Dietary Allowance (RDA) - 1,000mg for most adults and 1,200mg for women over 50 and men over 70 - the body pulls calcium from bones, weakening the skeleton and disrupting other systems.
Signs of deficiency often slip under the radar: mild muscle cramps, tingling in the fingers, or fatigue. In severe cases, it can lead to osteopenia, osteoporosis, or abnormal heart rhythms.
Understanding Hypertension
Hypertension is a chronic medical condition characterized by consistently elevated arterial pressure, typically defined as a systolic pressure of 130mmHg or higher, or a diastolic pressure of 80mmHg or higher. It’s a leading risk factor for heart attacks, strokes, and kidney disease. While genetics play a role, lifestyle factors such as sodium intake, physical inactivity, stress, and nutrient imbalances heavily influence its development.
How Calcium Influences Blood Pressure
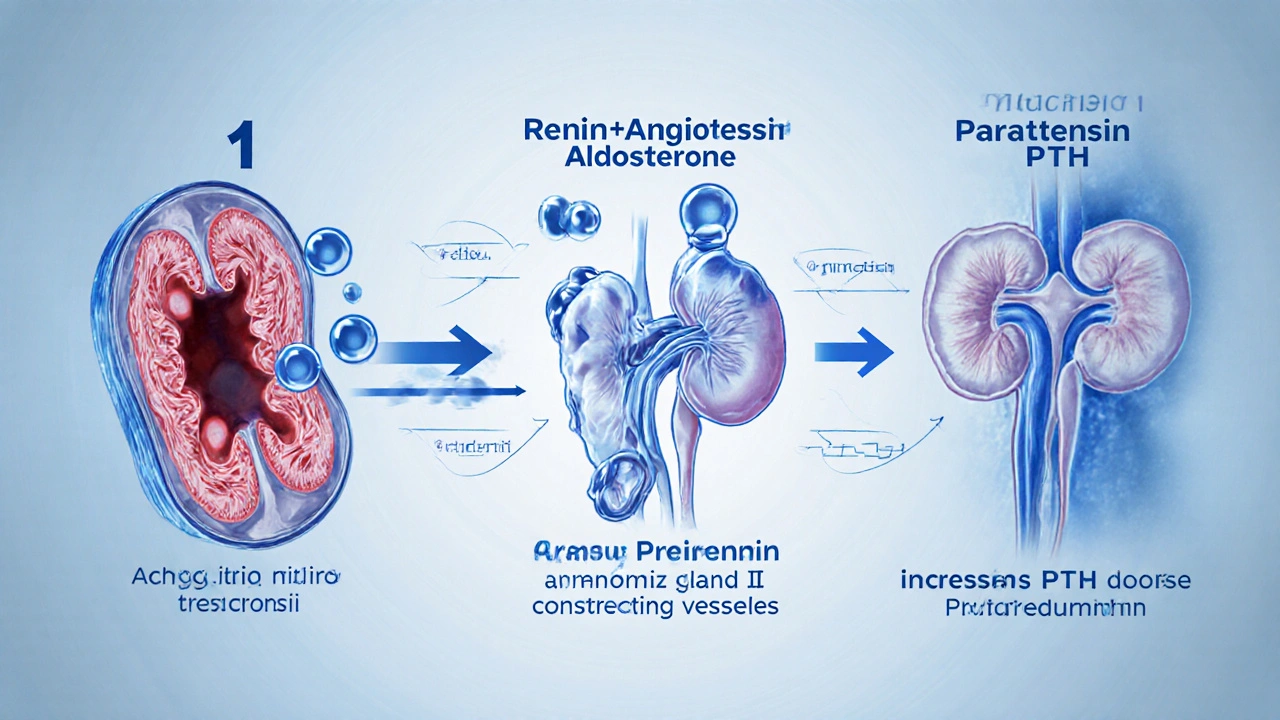
Three main mechanisms connect calcium status to blood‑pressure regulation:
- Vascular Smooth‑Muscle Tone: Calcium ions help muscle cells contract and relax. Low extracellular calcium causes blood vessels to stay more constricted, raising resistance and, consequently, pressure.
- Renin‑Angiotensin‑Aldosterone System (RAAS): Renin‑angiotensin system controls fluid balance and vasoconstriction. Insufficient calcium stimulates renin release, leading to higher angiotensinII levels and tighter vessels.
- Parathyroid Hormone (PTH) Activity: When calcium is low, the parathyroid glands secrete more parathyroid hormone, which raises blood calcium by pulling it from bones and enhancing kidney reabsorption of sodium. The extra sodium draws water into the bloodstream, increasing volume and pressure.
These pathways form a feedback loop: low calcium → higher PTH & renin → more sodium & vessel constriction → higher blood pressure.
What the Research Says
Multiple randomized controlled trials (RCTs) and meta‑analyses have examined calcium’s effect on hypertension.
- A 2022 meta‑analysis of 15 RCTs (over 12,000 participants) found that daily calcium supplementation of 1,200mg lowered systolic pressure by an average of 2.5mmHg and diastolic pressure by 1.2mmHg compared with placebo.
- The INTERMAP study (2007) linked dietary calcium intake of >1,000mg/day with a 4‑mmHg reduction in systolic pressure, independent of sodium consumption.
- In the DASH trial, participants on a high‑calcium diet (≈1,300mg) experienced a 5‑mmHg drop in systolic pressure compared to the control group, highlighting synergy with low sodium and high potassium.
While the numbers may seem modest, population‑wide shifts of even 2mmHg can prevent thousands of heart attacks and strokes each year.
Dietary Sources of Calcium
Getting enough calcium through food is generally safer and more effective than relying on pills. Below is a quick reference table:
| Food | Typical Serving | Calcium |
|---|---|---|
| Milk, 1 cup (240ml) | 1 cup | 300 |
| Yogurt, plain, 1 cup | 1 cup | 450 |
| Cheddar cheese | 1oz (28g) | 200 |
| Tofu (calcium‑set) | ½ cup | 350 |
| Almonds | ¼ cup | 100 |
| Broccoli, cooked | 1 cup | 60 |
| Salmon (canned with bones) | 3oz | 180 |
Notice how dairy products pack the most calcium per bite, but fortified plant milks, leafy greens, and fish with edible bones also contribute significantly.
Calcium Supplements: When and How to Use Them
Supplements are useful for people who can’t meet the RDA through food alone-such as vegans, lactose‑intolerant individuals, or older adults with reduced absorption.
- Type: Calcium carbonate (30% elemental calcium) requires stomach acid for absorption, best taken with meals. Calcium citrate (21% elemental calcium) is gentler on the stomach and can be taken anytime.
- Dosage: Split daily intake into two doses to improve absorption. Total supplemental calcium should not exceed 500mg if you already get 800‑900mg from diet.
- Safety: Excess calcium (≥2,500mg/day) raises the risk of kidney stones and may contribute to arterial calcification. Pair supplements with adequate magnesium and vitaminD to balance mineral metabolism.
Before starting any supplement, discuss with your healthcare provider, especially if you have a history of kidney disease or cardiovascular calcification.

Practical Strategies to Boost Calcium and Lower Blood Pressure
Here’s a simple 7‑day plan you can adapt:
- Start the day with a glass of fortified plant‑milk (≈300mg).
- Include a calcium‑rich snack like a small handful of almonds or a piece of cheese.
- Swap a soda for low‑sodium broth or herbal tea - reduces sodium while keeping you hydrated.
- Make half of your grains whole‑grain; they contain more magnesium, a mineral that works hand‑in‑hand with calcium.
- Pack a lunch featuring tofu stir‑fry or a salmon salad with bones; aim for at least 400mg at lunch.
- Dinner: a side of steamed broccoli or bokchoy, plus a cup of yogurt for dessert.
- Monitor your blood pressure each evening; note any changes after a week of increased calcium.
Pair this diet with 30minutes of moderate activity (walking, cycling) most days - exercise improves vascular elasticity and supports calcium metabolism.
Common Myths Debunked
- "More calcium always means lower blood pressure" - Only up to the RDA shows benefit; excess can backfire.
- "Only dairy matters" - Plant foods, fortified products, and fish are valuable sources.
- "Supplements are risk‑free" - High doses may cause kidney stones; always balance with magnesium and vitaminD.
Frequently Asked Questions
Can low calcium cause hypertension on its own?
Calcium deficiency alone rarely triggers high blood pressure, but it weakens the regulatory systems (RAAS and PTH) that keep pressure stable. Combined with high sodium intake, the effect becomes noticeable.
How much calcium should a hypertensive adult aim for?
The general recommendation is 1,200mg per day for adults over 50 and 1,000mg for younger adults. If you have hypertension, aiming for the upper end (1,200mg) can help modestly lower pressure, provided you keep sodium below 2,300mg.
Is calcium carbonate as effective as calcium citrate?
Both provide elemental calcium, but calcium citrate is absorbed better without stomach acid, making it preferable for older adults or those on acid‑reducing meds.
Do calcium‑rich diets increase the risk of arterial calcification?
When calcium intake stays within recommended limits and is paired with adequate vitaminD, magnesium, and a heart‑healthy diet, the risk is minimal. Problems arise mainly with over‑supplementation.
Can I replace calcium tablets with fortified orange juice?
Yes, if the juice is fortified with ≥300mg per cup and you drink it daily. Just watch the added sugars and ensure you’re not exceeding total calcium goals.
How quickly can blood pressure drop after increasing calcium intake?
Most studies show measurable reductions within 4‑8 weeks of consistent dietary changes. Immediate drops are uncommon; the effect builds gradually as hormonal balance normalizes.
Bottom Line
Calcium isn’t a magic bullet, but it’s a solid piece of the blood‑pressure puzzle. By meeting the recommended intake through diverse foods, keeping sodium low, and watching supplement doses, you give your heart a better chance to stay in the safe zone. Pair the diet with regular activity and routine blood‑pressure checks, and you’ll have a practical, evidence‑backed strategy to curb hypertension.

Jennifer Pavlik
October 8, 2025 AT 14:34Add a splash of fortified plant‑milk to your morning cereal – it’s an easy way to boost calcium without extra hassle.
Jacob Miller
October 15, 2025 AT 13:14Looks like the article tries to simplify a complex issue, but it forgets that most people don’t track every milligram of calcium they eat.
Anshul Gandhi
October 22, 2025 AT 11:54First, calcium’s role in vascular tone is well‑documented in peer‑reviewed journals, and no reputable study has ignored it. Second, the renin‑angiotensin system reacts to calcium levels faster than most people realize. Third, the parathyroid hormone surge triggered by low calcium is a direct pathway to sodium retention. Fourth, many of the so‑called “large‑scale” trials were funded by dairy lobbyists, which raises questions about bias. Fifth, independent meta‑analyses that exclude industry‑sponsored data still show a modest blood‑pressure drop, confirming the mechanism. Sixth, the effect size of 2‑3 mmHg may seem trivial, but epidemiologically it translates into thousands of prevented cardiovascular events. Seventh, the calcium‑sodium interaction is a hidden variable in most hypertension guidelines, and that omission is deliberate. Eighth, calcium supplements, when taken without magnesium and vitamin D, can actually increase arterial calcification, a fact hidden from the public. Ninth, the DASH diet’s success is partially due to its calcium content, not just potassium. Tenth, low‑dose calcium carbonate is poorly absorbed in older adults because of reduced stomach acid, a nuance the article glosses over. Eleventh, the recommended 1,200 mg per day for seniors is a compromise, not a hard rule, and many thriving centenarians live on less. Twelfth, excessive calcium intake above 2,500 mg is associated with kidney stones, a risk the piece barely acknowledges. Thirteenth, the interplay between vitamin K2 and calcium deposition in arteries is an emerging field, and ignoring it leads to oversimplification. Fourteenth, if you combine calcium tracking with regular ambulatory blood‑pressure monitoring, you can see personal trends more clearly. Fifteenth, in short, the article is a decent starter, but anyone serious about hypertension should dig deeper into the primary literature.
Emily Wang
October 29, 2025 AT 09:34If you’re looking for a quick win, swap one soda for a glass of fortified almond milk each morning. That simple swap adds roughly 300 mg of calcium and cuts a bit of sodium too. Pair it with a 10‑minute walk and you’ll notice your blood‑pressure cuff reading drop after a couple of weeks.
Hayden Kuhtze
November 5, 2025 AT 08:14Ah, another ‘miracle mineral’ post that pretends a sprinkle of calcium will solve all cardiovascular woes. The prose is as dense as cheese, yet the nuance is as thin as skim milk.
Craig Hoffman
November 12, 2025 AT 06:54Here’s the quick take – dairy gives the most calcium but fortified soy, tofu and leafy greens work too – keep total intake around 1,000‑1,200 mg a day and watch sodium.
Terry Duke
November 19, 2025 AT 05:34Wow!!! This article really breaks it down!!! Simple steps, clear tables, even a calculator – love it!!! 👍👍👍 Keep sharing these gems!!!
Chester Bennett
November 26, 2025 AT 04:14I appreciate the balanced overview; the inclusion of both dietary sources and the caution about over‑supplementation makes this a useful reference for anyone managing hypertension.
Emma French
December 3, 2025 AT 02:54Don’t overlook the importance of pairing calcium with magnesium – it’s essential for proper vascular function.
Debra Cine
December 10, 2025 AT 01:34Great summary! 🎉 Remember, a balanced plate with dairy or fortified alternatives can keep your calcium on track – and your heart will thank you! 😊
Rajinder Singh
December 17, 2025 AT 00:14Your exhaustive enumeration, while impressive, borders on theatrical hyperbole; nevertheless, the core truth remains – calcium’s influence on blood pressure is undeniable, and the public deserves a clearer, less sensationalized presentation.