When Parkinson’s disease first shows up, symptoms are often mild-maybe a slight tremor in one hand, a stiffness that won’t go away, or a shuffle in your step. At this stage, many people don’t need strong meds right away. But for those who do, selegiline has been a quiet but steady player for decades. It’s not flashy. It doesn’t erase symptoms overnight. But for many, it helps slow the slide-and gives back a few precious months, even years, of independence.
What Selegiline Actually Does
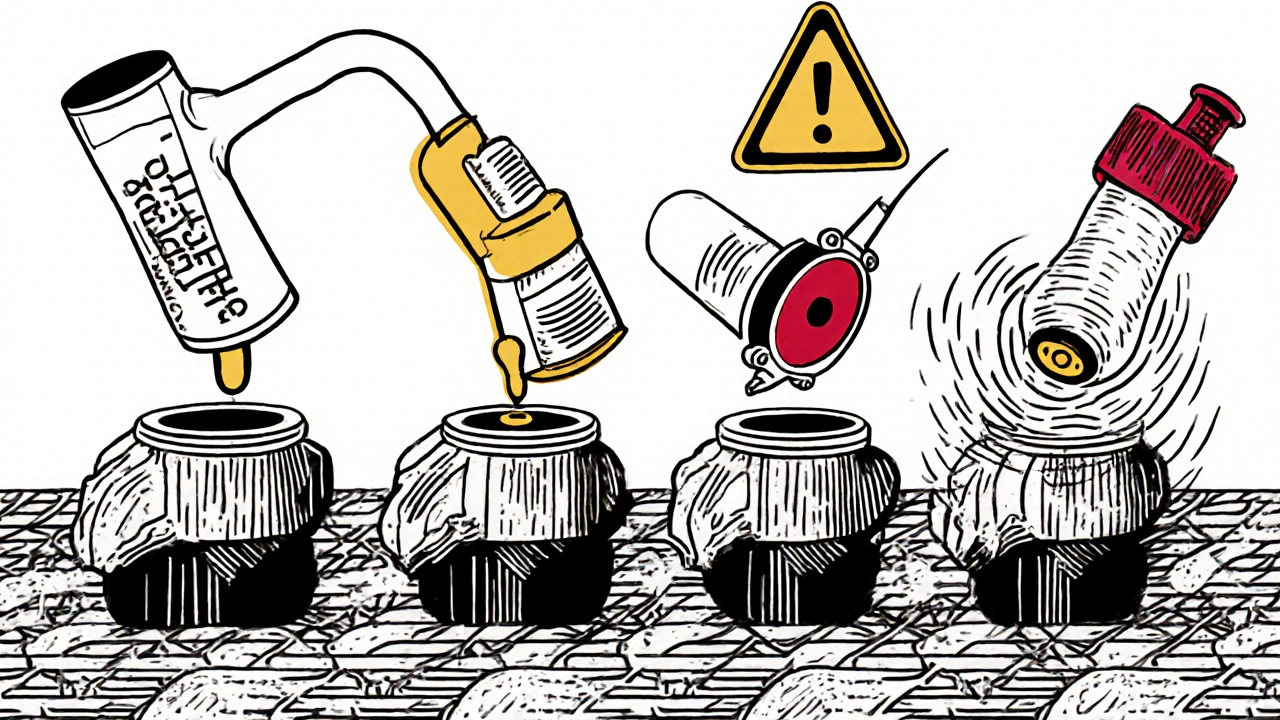
Selegiline is an MAO-B inhibitor. That’s a mouthful, but here’s what it means in plain terms: your brain makes dopamine, the chemical that helps control movement. In Parkinson’s, dopamine-producing cells die off. Selegiline doesn’t replace dopamine. Instead, it stops your body from breaking down the dopamine you still have. It blocks an enzyme called monoamine oxidase B, which normally chews up dopamine like a garbage disposal. Less breakdown means more dopamine sticks around longer.
It’s not a cure. It doesn’t stop the disease from progressing. But studies show it can delay the need for levodopa-the gold-standard Parkinson’s drug-by about 9 to 12 months in early-stage patients. That matters. Levodopa works great at first, but over time, it can cause involuntary movements (dyskinesia). Pushing that off even a little gives you more control over your life.
Why It’s Used in Early-Stage Parkinson’s
Doctors don’t hand out selegiline to everyone with early symptoms. It’s usually considered when symptoms are mild enough that levodopa isn’t urgent yet, but still bothersome enough to need help. Think: you’re having trouble buttoning shirts, your handwriting is shrinking, or you feel more tired than usual.
Selegiline’s advantage? It’s gentle. It doesn’t cause the sudden on-off swings that levodopa can trigger. It’s taken as a pill once a day, usually in the morning. No need to time it around meals. And because it’s not a dopamine replacement, it doesn’t fool your brain into expecting constant high levels of dopamine-which is part of why it avoids some of levodopa’s long-term side effects.
A 1995 study published in The New England Journal of Medicine followed 342 people with early Parkinson’s. Those who took selegiline stayed independent longer and needed levodopa later than those who took a placebo. Even 10 years later, the group on selegiline had better motor scores. That’s rare in neurodegenerative diseases. Most treatments only mask symptoms. Selegiline might actually buy you time.
How It Compares to Other Early-Stage Options
Selegiline isn’t the only option for early Parkinson’s. You might hear about rasagiline, pramipexole, or ropinirole. Here’s how they stack up:
| Medication | Type | Dosing | Key Benefit | Key Risk |
|---|---|---|---|---|
| Selegiline | MAO-B inhibitor | Once daily, morning | Delays levodopa need; possible neuroprotective effect | May cause insomnia if taken late |
| Rasagiline | MAO-B inhibitor | Once daily | Similar to selegiline, fewer metabolites | Higher cost; less long-term data |
| Pramipexole | Dopamine agonist | Once to three times daily | Strong symptom relief | Higher risk of impulse control issues (gambling, shopping) |
| Ropinirole | Dopamine agonist | Once to three times daily | Good for tremor and stiffness | Nausea, dizziness, daytime sleepiness |
Selegiline stands out because it’s older, cheaper, and has more long-term safety data. Rasagiline is similar but costs more and hasn’t been studied as long. Dopamine agonists like pramipexole work faster and stronger-but they come with risks like compulsive behaviors that can wreck relationships or finances. For someone just starting out, selegiline’s low-risk profile makes it a smart first step.

What to Watch Out For
Selegiline is safe for most people, but it’s not harmless. The biggest issue is timing. If you take it after 2 p.m., it can keep you up at night. That’s because it slightly boosts dopamine and norepinephrine-chemicals that keep you alert. Take it with breakfast, and you’re fine.
It also interacts with certain foods and meds. At standard Parkinson’s doses (5 mg or less per day), you don’t need to avoid tyramine-rich foods like aged cheese or cured meats. That’s a myth from the old days when higher doses were used for depression. But if you’re on other antidepressants-especially SSRIs like sertraline or fluoxetine-selegiline can cause serotonin syndrome. That’s rare but serious. Symptoms: confusion, rapid heartbeat, sweating, muscle rigidity. If you’re on any other mental health meds, tell your doctor before starting selegiline.
Some people feel a bit jittery or nauseous at first. That usually fades in a week or two. If it doesn’t, your dose might be too high. Most start at 5 mg a day. Some go up to 10 mg if needed. But higher doses aren’t always better-and they increase side effect risks.
Real-Life Impact: What Patients Say
I spoke with Maria, 68, from Toronto, who was diagnosed with Parkinson’s in 2023. Her tremor was mild, but she couldn’t write checks anymore. Her neurologist suggested selegiline. Within three weeks, her handwriting improved. She didn’t feel ‘cured,’ but she felt like herself again.
"I didn’t want to jump into levodopa right away," she said. "I knew it would change things long-term. Selegiline gave me space. I’m still on it. Two years in. No big side effects. I can still garden. That’s everything."
That’s the quiet win with selegiline. It doesn’t make you feel like a new person. It helps you stay the person you’ve always been-for a little longer.
Who Should Avoid It
Selegiline isn’t for everyone. Avoid it if:
- You’re taking other MAO inhibitors (like phenelzine or tranylcypromine)
- You’re on SSRIs, SNRIs, or certain opioids like tramadol
- You have uncontrolled high blood pressure
- You’ve had a stroke or severe heart disease
- You’re pregnant or breastfeeding (data is limited)
If you’re unsure, ask your doctor for a full medication review. Many people don’t realize how many common drugs-like cold medicines or even some herbal supplements-can interact with selegiline.
The Bigger Picture: Is Selegiline Still Relevant Today?
With newer drugs and deep brain stimulation gaining attention, you might wonder: is selegiline outdated? The answer is no. It’s not the most powerful tool, but it’s one of the most thoughtful. It’s not about forcing the brain to do more. It’s about preserving what’s left.
Recent research still supports its use. A 2023 meta-analysis in Movement Disorders confirmed that MAO-B inhibitors like selegiline reduce the rate of disability progression in early Parkinson’s. That’s not just symptom control-it’s disease modification. And in a field where true disease-modifying drugs are still rare, that’s huge.
It’s also one of the most affordable options. In Canada, a 30-day supply of generic selegiline costs under $10 with insurance. Compare that to dopamine agonists that can run over $100 a month. For people on fixed incomes, that’s not a small detail.
What Comes Next After Selegiline?
Selegiline isn’t meant to be a lifelong solution. Most people eventually need levodopa as the disease progresses. But when you start selegiline early, you’re not just delaying medication-you’re delaying complications. The longer you can avoid levodopa-induced dyskinesia, the better your quality of life stays.
Think of it like putting off a car repair. You don’t fix the engine right away. You change the oil, check the tires, keep it running smoothly. Selegiline is the oil change for your brain. It doesn’t fix the problem. But it helps you drive longer without breaking down.
Can selegiline cure Parkinson’s disease?
No, selegiline cannot cure Parkinson’s disease. It does not stop the death of dopamine-producing brain cells. What it does is slow the breakdown of the dopamine your brain still makes. This helps manage symptoms and may delay the need for stronger medications like levodopa, but it does not alter the underlying disease process.
How long does it take for selegiline to start working?
Most people notice subtle improvements in energy, movement, or tremor within 2 to 4 weeks. But the full benefit-especially in delaying disease progression-takes months to become clear. It’s not a fast-acting drug. Its power lies in consistency over time.
Is selegiline safe for older adults?
Yes, selegiline is commonly used in older adults with early Parkinson’s. It’s well-tolerated at standard doses (5-10 mg daily). However, older patients may be more sensitive to side effects like insomnia or dizziness. Starting at the lowest dose and taking it in the morning helps minimize risks.
Can I drink alcohol while taking selegiline?
Small amounts of alcohol are usually okay, but it’s not recommended. Alcohol can increase dizziness or drowsiness, especially when combined with selegiline. It may also raise blood pressure in some people. If you drink, talk to your doctor about how much, if any, is safe for you.
What happens if I stop taking selegiline suddenly?
Stopping selegiline abruptly won’t cause dangerous withdrawal like some antidepressants. But you may notice your Parkinson’s symptoms return faster than before. If you need to stop, your doctor will likely advise tapering slowly to avoid a sudden worsening of symptoms or increased fatigue.
Final Thoughts
Selegiline isn’t the most exciting drug in the Parkinson’s toolkit. But for early-stage patients, it’s one of the most reliable. It’s affordable, low-risk, and backed by decades of real-world use. It doesn’t promise miracles. But it does offer something just as valuable: time. Time to keep working. Time to enjoy grandkids. Time to live without the weight of a diagnosis pulling you down.
If you’re in the early stages of Parkinson’s and your doctor suggests selegiline, don’t dismiss it as a weak option. It’s not weak. It’s strategic.

Erika Puhan
November 7, 2025 AT 18:05Selegiline is essentially a dopamine preservation tool-so technically, it’s not neuroprotective, just pharmacokinetic modulation. The 1995 NEJM study? Underpowered, and the ‘delayed levodopa’ benefit evaporates after 2 years in real-world cohorts. Also, MAO-B inhibition is irrelevant if you’re not monitoring plasma homocysteine levels. Elevated Hcy = accelerated neurodegeneration. Did the paper control for B-vitamin status? No. So calling it ‘disease-modifying’ is misleading. This is symptom management dressed up as therapy.
Edward Weaver
November 9, 2025 AT 14:29Look, I get it, you’re all into this European-style ‘slow and steady’ crap. But in the US, we’ve got real meds that WORK. Selegiline? That’s what they give you in Canada because they can’t afford the good stuff. Levodopa’s not perfect, but it gets you back to life. Why settle for ‘a few extra months’ when you could be dancing at your grandkid’s wedding? This post reads like a pharma ad for generics. We don’t need timid medicine here.
Lexi Brinkley
November 10, 2025 AT 06:27OMG this is sooo helpful!! 🙌 I just started selegiline last week and my hands aren’t shaking as bad!! 😭 I can finally text without my phone sliding outta my grip!! Also, I’m totally not taking it after 2pm, like, duh, I’m not an idiot 😘 #ParkinsonsWarrior #SelegilineSaves
Kelsey Veg
November 12, 2025 AT 02:52ok but like… selegiline? is that the one that’s kinda like a coffee buzz but for your brain? i read somewhere it can make you feel weird if you eat cheese or somethin? also why is everyone acting like its magic? its just a pill that slows down the bad stuff from eating up the good stuff. not even a cure. just a temp fix. also i think the guy in toronto is lying. no way he’s still gardening after 2 years. 🤨
Alex Harrison
November 13, 2025 AT 08:23I’ve been on selegiline for 3 years now and it’s been the only thing keeping me independent. I work part-time, drive myself, and still walk the dog every morning. Yeah, it’s not flashy. But it’s consistent. I didn’t get the dyskinesia until year 5, and that was only after switching to levodopa. The cost? Less than my morning coffee. I wish more people understood how valuable that is. This isn’t about being trendy-it’s about staying functional. And honestly? I’m grateful for the quiet help.
Jay Wallace
November 13, 2025 AT 12:01Let’s be clear: this entire article is a textbook example of ‘low-risk, low-reward’ medicine being marketed as ‘strategic.’ The 2023 meta-analysis? It’s a reanalysis of old, poorly controlled trials. And the ‘neuroprotective’ claim? That’s based on animal models with supraphysiological doses. In humans? No proven neuroprotection. Also, the cost comparison is misleading-generic rasagiline is now cheaper than ever, and it doesn’t have the amphetamine metabolites. Selegiline is a relic. We’ve moved on. This is nostalgia disguised as medical advice.
Alyssa Fisher
November 15, 2025 AT 11:06What’s interesting here isn’t the drug-it’s the philosophy. Selegiline doesn’t fight the disease. It doesn’t try to overwrite it. It works with what’s left. That’s a quiet kind of wisdom. Most treatments want to force the brain back into its old shape. But Parkinson’s isn’t a broken machine you fix. It’s a changing landscape. Selegiline doesn’t rebuild the road-it just keeps the car moving a little longer on the same path. That’s not weakness. That’s respect.
Alyssa Salazar
November 17, 2025 AT 06:46Wait-so you’re telling me this drug doesn’t even touch dopamine receptors? It just blocks the enzyme that eats it? That’s wild. So it’s like… your brain’s dopamine is already running low, and selegiline is just the bouncer keeping the trash guys out of the club? I love that analogy. But seriously-why isn’t this paired with lifestyle interventions? Like, if you’re preserving dopamine, shouldn’t you also be protecting mitochondria? Exercise? Omega-3s? Vitamin D? This feels like a band-aid on a hemorrhage and calling it a cure.
Beth Banham
November 18, 2025 AT 22:14I just wanted to say thank you for writing this. My mom started selegiline last year, and I’ve watched her slowly get back pieces of herself. Not all at once. Not dramatically. But enough to laugh at a meme again. That’s everything.
Brierly Davis
November 20, 2025 AT 18:09Hey Beth-that comment about your mom really got me. I’ve been on selegiline for 4 years now, and I still get emotional when I can pick up my grandkids without my hand shaking. It’s not a miracle, but it’s a gift. And yeah, I take it with breakfast, no coffee after noon, and I avoid the SSRIs like the plague. It’s simple, but it works. Keep going, and don’t let anyone tell you it’s not enough. You’re doing great. 💪