Every year, millions of Canadians and Americans pay hundreds or even thousands of dollars extra for brand-name drugs-when a cheaper, just-as-effective generic version is sitting right there in the pharmacy’s back room. The problem isn’t that generics are hard to find. It’s that most people don’t know how to ask for them-or even if they’re available.
If your doctor wrote a prescription for, say, Prilosec, you might assume that’s the only option. But omeprazole is the generic version. It does the same thing. It’s been approved by Health Canada and the FDA. And it costs about 90% less. The same goes for Lipitor (atorvastatin), Zoloft (sertraline), Viagra (sildenafil), and dozens more. The question isn’t whether a generic exists. It’s whether you’ve checked.
Why Generics Are Just as Safe (and Often Better)
There’s a myth that generics are "inferior" or "weaker." That’s not true. The FDA requires generics to have the exact same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also be bioequivalent-meaning your body absorbs them at the same rate and to the same extent, within a 80-125% range. That’s not a loophole. That’s science.
Take levothyroxine, a thyroid medication. Some patients worry about switching between brands because tiny changes in absorption can affect how they feel. That’s why pharmacists are trained to stick with the same generic manufacturer if you’ve been stable on one. But switching from brand to generic-or between two AB-rated generics-is still considered safe by the FDA and Health Canada. The real issue isn’t safety. It’s awareness.
According to the FDA, 90% of all prescriptions in the U.S. are filled with generics. In Canada, the rate is similar. Yet, only 32% of patients can correctly identify when a generic is truly equivalent. Most don’t know the difference between a generic and a brand. Or worse-they think they’re being "cheated" when they get a different-looking pill.
How to Check for a Generic Version
You don’t need a medical degree. You don’t need to dig through legal documents. Here’s how to find out if your prescription has a cheaper alternative.
- Ask your pharmacist directly-not "Do you have a generic?" but "Is there a therapeutically equivalent generic available for this prescription?" Pharmacists are trained to know this. In fact, a 2022 study in JAMA Internal Medicine found they correctly identify generic alternatives 98.7% of the time. CVS, Walgreens, and Shoppers Drug Mart all have systems that automatically flag generics when you fill a prescription. They’ll tell you before you pay.
- Check your insurance formulary-If you’re on a drug plan (like OHIP+ in Ontario, or a private plan), log into your insurer’s website. Search for your brand-name drug. If a generic is covered, it’ll say so. Many plans require you to try the generic first before approving the brand. That’s not a restriction-it’s a savings tool.
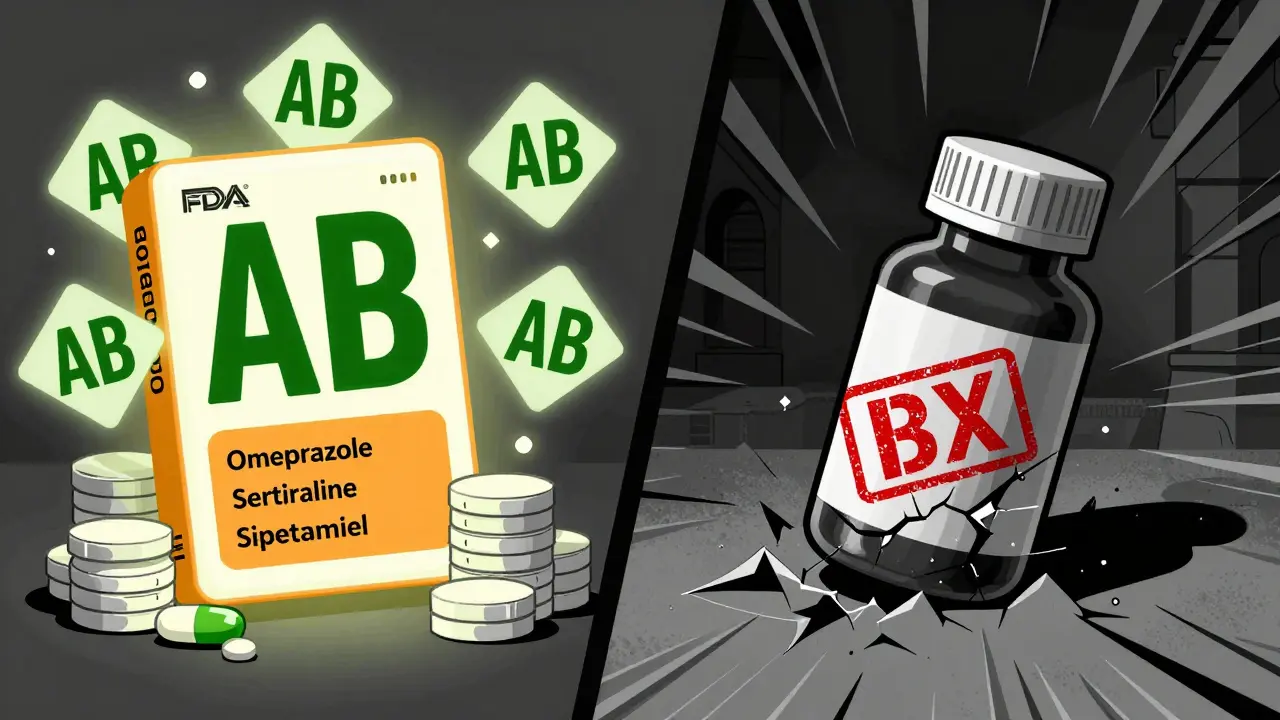
- Use the FDA’s Drugs@FDA database-Type in your brand-name drug (like "Lipitor") on Drugs@FDA. Look for the "Therapeutic Equivalence Code." If it says "AB," that means it’s rated interchangeable with the brand. "BX" means it’s not recommended for substitution. This is the gold standard. It’s free. And it’s updated daily.
- Try GoodRx or Canada’s Drug Prices-These sites compare prices across pharmacies. But don’t just look at the cost. Click through to see if the price is for the generic or brand. GoodRx shows both. If you see a $15 price for atorvastatin and a $765 price for Lipitor, you know what to ask for.
- Check your prescription label-Sometimes, the pharmacy already substituted the generic and printed it on the label. Look for the drug name. If it says "atorvastatin" instead of "Lipitor," you’re already on the cheaper version.
What the Orange Book Means (And How to Read It)
The FDA’s "Orange Book" is the official list of all approved drugs with therapeutic equivalence ratings. It’s not a secret document. It’s public. And it’s the key to knowing if a generic is truly interchangeable.
Each generic gets a two-letter code:
- AB = Fully equivalent. Safe to substitute.
- AP = Approved, but not yet rated (usually new generics).
- BN = Brand-name only, no generic available.
- BX = Not recommended for substitution. Often because of complex delivery systems (like inhalers or patches).
For example, if your prescription is for Advair Diskus (fluticasone/salmeterol), you’ll see a "BX" rating. That’s because inhalers are hard to replicate exactly. But if you’re on Metformin, you’ll see "AB"-and you can safely switch to any generic.
Most people don’t know this exists. But pharmacists do. So if you’re unsure, ask: "Is this drug rated AB in the Orange Book?"
When Generics Might Not Be the Best Choice
There are exceptions. For drugs with a narrow therapeutic index-where even a small change in blood levels can cause harm-doctors sometimes prefer to stick with one brand or generic. These include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid)
- Phenytoin (seizure medication)
- Cyclosporine (organ transplant)
In these cases, consistency matters more than cost. If you’ve been stable on one version, switching might cause side effects. That’s why your doctor might write "Do Not Substitute" on the prescription. But even then, you can still ask: "Is there a generic version that’s been stable for other patients?" Sometimes, the answer is yes.
What to Do If Your Pharmacy Refuses to Switch
Sometimes, pharmacies won’t automatically switch-even when a generic exists. Reasons vary:
- Your insurance requires prior authorization for the brand.
- The pharmacy doesn’t stock the generic.
- The doctor didn’t allow substitution.
If you’re being charged full price for a brand when a generic is available, here’s what to do:
- Ask the pharmacist to check their inventory. Many generics are stored in back rooms and not on the shelf.
- Request a 30-day trial of the generic. Most people tolerate it just fine.
- If they say "It’s not covered," ask for a formulary exception. Many plans will approve it if you show the cost difference.
- Call your doctor’s office. Sometimes, they just need to update the prescription to "dispense as written" or "substitution allowed."
Don’t accept "We don’t have it" as the final answer. Ask them to order it. Most can get a generic within 24 hours.
How Much Can You Really Save?
Let’s put numbers to it.
In 2022, the average retail price for a brand-name drug in the U.S. was $765.09. The average generic? $15.23. That’s a 98% difference.
In Canada, the gap is smaller but still huge. A 30-day supply of Simvastatin (generic for Zocor) costs about $12 at Shoppers Drug Mart. The brand version? $140. That’s $1,500 a year saved.
One Reddit user in Toronto shared that switching from brand-name Lexapro to generic escitalopram cut his monthly cost from $110 to $15. He saved $1,140 a year. That’s a vacation. A new pair of shoes. A month’s worth of transit passes.
And you don’t need to be rich to benefit. Even if you’re on a government drug plan, switching to a generic can free up your annual limit for other medications.
What’s Changing in 2024
Things are getting easier. As of January 1, 2024, Medicare Part D plans in the U.S. are required to show real-time generic availability on their online tools. Canada’s public drug plans are following suit.
The FDA just launched a simpler version of Drugs@FDA designed for patients-not pharmacists. It now has a "Generic Drug Search" button that lets you type in a brand name and instantly see if a generic exists, what it’s called, and how much it costs.
Pharmacy chains are also updating their systems. By Q3 2024, Epic EHR (used by most hospitals and clinics) will automatically alert doctors when a generic is available and appropriate. That means the next time your doctor writes a prescription, the system might pop up: "A generic version of this drug is available and costs 90% less. Would you like to switch?"
This isn’t a future idea. It’s happening now.
Final Tip: Don’t Be Afraid to Ask
The biggest barrier to saving money on prescriptions isn’t technology. It’s silence. People don’t ask because they’re embarrassed, intimidated, or think it’s not their place.
But here’s the truth: Your pharmacist is paid to help you save money. Your doctor wants you to take your meds. Your insurance company wants you to stay healthy and spend less.
Next time you pick up a prescription, say: "Is there a generic version of this? And if so, can I switch to it?"
It takes 30 seconds. It could save you hundreds. And you’re not asking for a favor-you’re asking for a right.

Daniel Pate
January 13, 2026 AT 08:29Most people don’t realize generics are legally required to be bioequivalent. The FDA doesn’t just slap a label on a pill and call it good. There are strict tests-dissolution rates, plasma concentration curves, you name it. If it’s AB-rated, it’s the same drug, period. The only time I’ve seen issues is with thyroid meds, and even then, it’s usually because someone switched manufacturers three times in a year. Stick with one generic, and you’re fine.
Amanda Eichstaedt
January 13, 2026 AT 16:49I used to think generics were for people who couldn’t afford the real thing. Then I switched from Lexapro to escitalopram and didn’t notice a difference-except my bank account. My therapist didn’t even blink when I told her. It’s not about quality, it’s about marketing. Brand names spend billions on ads; generics spend it on making the pill cheaper.
Eileen Reilly
January 14, 2026 AT 00:59Ugh another one of these posts. Like we dont all know generics are cheaper. But guess what? Sometimes the generic gives me nausea, the brand doesnt. So yeah, I pay the extra $70 a month because my body isnt a lab rat. And no, I dont care if you think Im dumb for it. I feel better. Thats the point.
Cecelia Alta
January 14, 2026 AT 16:24Oh wow, let me get this straight-your pharmacist is now your primary care physician, your insurance is your pharmacist, and your doctor is just the guy who writes the order? And you think this is empowerment? No. This is a system designed to shift responsibility onto patients who have zero training in pharmacology. You’re being told to become an expert on Orange Book codes just to get your blood pressure meds. That’s not access, that’s exploitation dressed up as savings.
And don’t get me started on GoodRx. It’s a middleman that profits off your desperation. They’re not saving you money-they’re selling your data to pharma so they can raise prices later. You’re not a consumer. You’re a data point.
Faith Wright
January 14, 2026 AT 22:25Can we just talk about how ridiculous it is that we have to do this? You shouldn’t need a 5-step checklist just to get a pill that works the same as the one your doctor prescribed. This isn’t a hack. This isn’t a tip. This is a broken system where the only people who benefit are the ones who don’t need to ask.
I used to work at a pharmacy. People would cry because they couldn’t afford their brand-name insulin. Meanwhile, the generic was sitting in the back, and the pharmacist had to beg the doctor to change the script. No one should have to beg for basic healthcare.
Rebekah Cobbson
January 15, 2026 AT 02:37I love that this post includes the Orange Book codes. Most people don’t even know that exists. But here’s the thing-if you’re on a chronic medication and you’re stable, don’t switch unless you have to. And if you do switch, give it a full month. Your body needs time to adjust. And if you feel off? Go back. No shame. Your health isn’t a budget spreadsheet.
Also, if your pharmacy says "we don’t have it," ask them to order it. Most can get it overnight. Don’t settle for "it’s not on the shelf." That’s not service-that’s laziness.
Audu ikhlas
January 15, 2026 AT 09:58Why are you all so obsessed with American drugs? In Nigeria we dont even have generics, we have fake pills sold on the street. You think your $15 pill is safe? Maybe. But here we dont even have the luxury of asking. You people complain about $140 for Zocor? We pay $300 for fake metformin that gives us liver failure. Stop acting like this is a privilege.
Sonal Guha
January 15, 2026 AT 10:42Generics are fine unless you have a narrow therapeutic index then its a gamble. Levothyroxine is not a joke. One study showed 30 of patients had TSH fluctuations after switching. So dont tell me its the same. Its not. And dont tell me to ask my pharmacist. They dont know what TSH means.
TiM Vince
January 15, 2026 AT 10:54My dad was on Lipitor for 12 years. Switched to atorvastatin after his Medicare plan forced it. He was worried. We checked the FDA database together. AB rating. Same dose. Same everything. He’s been on it for 5 years now. No side effects. Saved $1,200 a year. He says he’s not a cheapskate-he’s just smart.
gary ysturiz
January 15, 2026 AT 14:43If you’re paying full price for a brand-name drug and you don’t know if a generic exists-you’re not being loyal. You’re being overcharged. It’s not complicated. Ask. Check. Switch. Save. Repeat. No drama. No guilt. Just common sense.
Jessica Bnouzalim
January 15, 2026 AT 15:09OMG I just realized I’ve been on generic sertraline for 3 years and I thought it was Zoloft because the bottle looked the same?? I’m so embarrassed. But also-YESSSSS. I saved like $90 a month?? My cat now has a new scratching post and I didn’t even have to skip coffee. This post changed my life. Thank you thank you thank you!!
laura manning
January 16, 2026 AT 01:38It is imperative to note, however, that the therapeutic equivalence ratings referenced herein are subject to revision by the Food and Drug Administration on a biweekly basis, and the Orange Book, while authoritative, does not account for inter-manufacturer variability in inactive ingredients, which may, in rare but documented cases, precipitate clinically significant pharmacokinetic deviations in patients with comorbid gastrointestinal disorders or hepatic impairment. Therefore, while the general recommendation to utilize generics is statistically sound, individualized clinical judgment remains paramount.