When your prescription runs out and the pharmacy says it’s out of stock
You show up for your refill, and the pharmacist says, "Sorry, we’re out." Not just out for a day - out for weeks. Maybe even months. This isn’t rare anymore. In 2025, over 258 different active drug ingredients were in short supply across the U.S., affecting nearly 2,000 prescription medications. Insulin, antibiotics, chemotherapy drugs, even basic pain relievers like acetaminophen injections - all have hit critical shortages. And when your medicine disappears, panic sets in. But there are steps you can take - and they’re not as complicated as you think.
First, don’t stop taking your medication
It’s tempting. You’re scared. You don’t know what to do. So you skip doses. You cut pills in half. You wait it out. But stopping your medicine without guidance can be dangerous. Blood pressure spikes. Blood sugar crashes. Seizures return. One survey found that 32% of patients stopped their meds during shortages - and half of them ended up in the ER or needed urgent care. That’s not a risk worth taking.
Instead, call your doctor. Don’t wait. Don’t assume they know about the shortage. Many don’t. Your doctor needs to know you’re affected so they can act. They might switch you to another drug in the same class, adjust your dose, or prescribe a different formulation - like switching from an injection to a pill if possible.
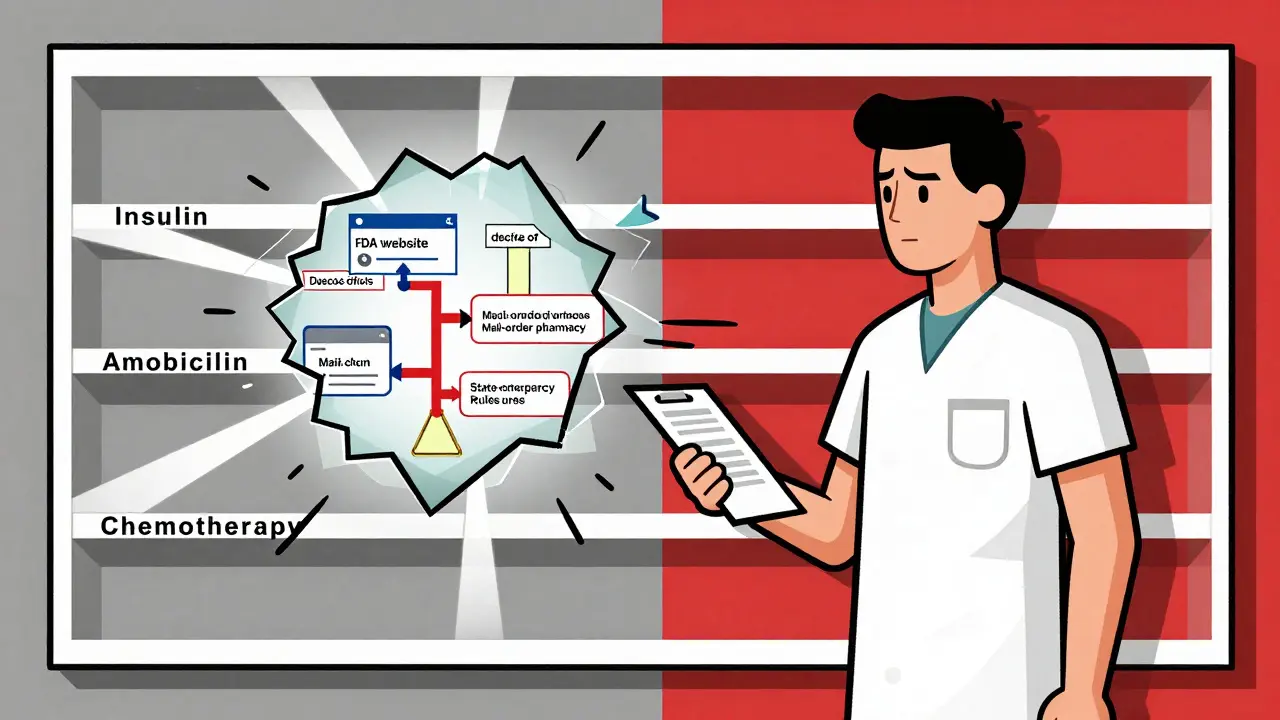
Check the FDA’s drug shortage list
The FDA keeps a public, updated list of all active drug shortages. It’s not perfect - it doesn’t tell you what’s in stock at your local pharmacy - but it tells you what’s missing and what alternatives are approved. For example, during the Semglee insulin shortage in March 2025, the FDA confirmed that Lantus could be substituted without a new prescription because Semglee is an interchangeable biosimilar. That’s huge. It means your pharmacist can swap them without waiting for your doctor to sign off.
Go to fda.gov/drugshortages and search for your drug. If it’s listed, look under "Alternatives". You’ll see what other drugs are considered therapeutically equivalent. Don’t ignore this step. It’s your first real clue on what’s safe to use.
Call more than one pharmacy
One pharmacy saying "no" doesn’t mean all pharmacies are out. In fact, during the Semglee shortage, one Reddit user, DiabeticDad87, contacted seven different pharmacies over three days before finding a supply. Some chains have better inventory than others. Mail-order pharmacies often have larger stockpiles. Independent pharmacies sometimes get shipments before big chains. And don’t forget specialty pharmacies - they handle complex meds like cancer drugs and injectables.
Pro tip: Ask if they’re on a waitlist. Many pharmacies keep lists for patients needing shortage drugs. When stock arrives, they call you. You might get it sooner than you think.

Ask about therapeutic alternatives - not just brand swaps
Not all alternatives are the same. Switching from one insulin to another isn’t like swapping coffee brands. Dosing, timing, and how your body reacts matter. But sometimes, a different drug in the same class works just as well.
For example, during amoxicillin shortages, doctors turned to azithromycin for certain infections. But azithromycin isn’t a perfect replacement - it works differently, has different side effects, and can contribute to antibiotic resistance if used carelessly. Your doctor needs to know the reason you’re taking the drug before suggesting a swap.
For chronic conditions like autoimmune diseases, some patients saw their treatment duration cut from 100+ days to just a few days during shortages. That’s not ideal, but it kept people alive. Your doctor might lower your dose temporarily or extend the time between doses. These aren’t perfect solutions, but they’re safer than stopping.
Know your insurance’s rules
Even if a drug is medically appropriate, your insurance might not cover it. During the Semglee shortage, Blue Cross NC changed its formulary rules: Lantus became covered without prior authorization on some plans. That’s a big deal. But you won’t know unless you ask.
Call your insurer. Ask: "Is there a covered alternative to [your drug]?" and "Has my plan changed its rules for this drug due to the shortage?" Some insurers have special exceptions during shortages. Others require paperwork. Either way, you need the info before your doctor writes a new prescription.
State-level solutions are changing the game
Some states are stepping in where federal systems fall short. New Jersey proposed letting pharmacists hand out emergency insulin supplies without a prescription during shortages. Hawaii approved using drugs approved in other countries - like Canada or the EU - if they’re safe and meet standards. California, New York, and Massachusetts are stockpiling critical drugs like abortion medications and chemotherapy agents to guard against political or supply chain disruptions.
These aren’t national policies - yet. But if you live in one of these states, you have more options. Check your state’s board of pharmacy website. They often post updates on emergency substitution rules.
Don’t trust random online sources
Reddit threads, Facebook groups, and YouTube videos might tell you about "secret" alternatives or how to order from overseas pharmacies. Some of that advice is helpful. But a lot of it is dangerous. Ordering drugs from unregulated websites can land you with fake, contaminated, or expired medicine. The FDA has cracked down on illegal online pharmacies selling insulin and cancer drugs - and people have died.
If you’re desperate, talk to your pharmacist. They know the legal options. Most major chains now have shortage specialists you can schedule a 15-minute call with. It’s free. And they’ve helped hundreds of people just like you.
What about generics? Are they safe?
Yes - but not always. Generic drugs are required to be bioequivalent to brand-name versions. But during shortages, the same few manufacturers make most generics. In fact, 85% of generic drugs come from just five companies. If one plant has a quality issue - like contamination or equipment failure - dozens of drugs vanish at once.
That’s why insulin shortages hit so hard. Semglee, Lantus, Basaglar - they’re all made by the same few factories. When one shuts down, all of them feel it. That’s why alternatives matter. Sometimes, switching to a different brand - even if it’s more expensive - is the only way to keep your treatment going.
How long do shortages last?
Most don’t end quickly. Of the shortages that started between 2018 and 2023, 75% lasted over a year. More than half lasted two years or longer. This isn’t a temporary glitch. It’s a broken system.
But there’s progress. Since January 2025, the FDA has increased inspections at critical drug manufacturing sites from quarterly to monthly. That’s already cut new shortages by 15%. Health systems are testing real-time tools that alert doctors to shortages the moment they’re prescribing - and suggest alternatives on the spot. Early results show a 28% faster switch to safe alternatives.
What you can do today
- Call your doctor and tell them you can’t get your medication.
- Check the FDA Drug Shortage Database for your drug and approved alternatives.
- Call at least three pharmacies - including your mail-order provider.
- Ask your insurer if they’ve changed coverage rules for your drug or its alternatives.
- Ask your pharmacist if they offer shortage counseling - most do now, for free.
You’re not alone. Thousands of people are in the same boat. The system is failing - but you still have control. You don’t have to guess. You don’t have to risk your health. You just need to ask the right questions - and keep pushing until you get answers.
When to worry
Some shortages are more urgent than others. If you’re taking:
- Insulin - missing doses can lead to diabetic ketoacidosis, a life-threatening emergency
- Chemotherapy drugs - delays can reduce treatment effectiveness
- Anti-seizure meds - skipping doses can trigger seizures
- Heart medications like beta-blockers or blood thinners - stopping suddenly can cause heart attacks or strokes
If you’re on any of these, call your doctor immediately. Don’t wait for your refill. Don’t hope it comes back. Act now.