Chronic diarrhea that won’t go away-even after trying probiotics, cutting out dairy, or switching diets-can be more than just an annoying inconvenience. For many people, especially women over 50, it’s a sign of microscopic colitis, a hidden inflammation in the colon that doesn’t show up on a regular colonoscopy. You can look perfectly normal inside, but under the microscope, the tissue tells a different story. And if you’ve been suffering for months or even years without a diagnosis, you’re not alone. The average time from first symptoms to diagnosis is 11 months. But once you know what’s going on, there’s a clear, effective path forward: budesonide.
What Exactly Is Microscopic Colitis?
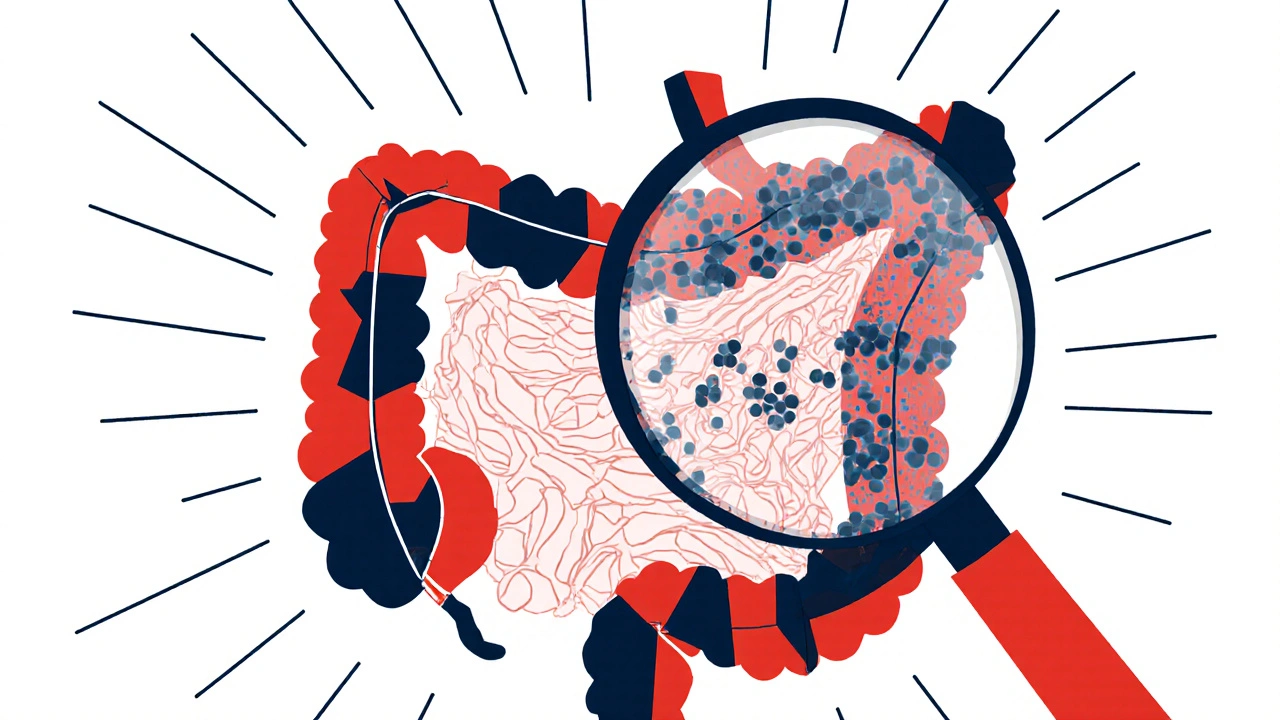
Microscopic colitis (MC) is an inflammatory condition of the colon that causes persistent, watery, non-bloody diarrhea. Unlike Crohn’s disease or ulcerative colitis, there’s no visible damage during a colonoscopy. The colon looks healthy to the naked eye. That’s why it’s called microscopic-you need a biopsy, looked at under a microscope, to see the problem.
There are two main types: collagenous colitis and lymphocytic colitis. In collagenous colitis, a thick band of collagen-like scar tissue-builds up just beneath the surface lining of the colon. In lymphocytic colitis, there’s an overgrowth of white blood cells (lymphocytes) inside the lining. Both disrupt the colon’s ability to absorb water, leading to frequent, urgent bowel movements-often 5 to 10 times a day.
It’s more common in women, making up 65 to 70% of cases. Most people are diagnosed in their 60s, though it can happen at any age. The condition often comes and goes in cycles, with symptoms lasting months or even years before someone finally gets tested. Many patients report abdominal cramps, weight loss, fecal incontinence, and even nighttime diarrhea. It’s not just inconvenient-it’s life-limiting.
Why Diagnosis Is So Often Delayed
Because the colon looks normal during a scope, doctors often assume it’s irritable bowel syndrome (IBS), food intolerance, or even stress. Many patients are told to try a low-FODMAP diet, take loperamide, or avoid caffeine. When those don’t work, they’re sent for more tests-sometimes years later.
The key is knowing when to push for a biopsy. If you’ve had chronic watery diarrhea for more than 4 weeks-with no blood, no fever, no weight loss that screams infection-it’s time to ask for colonic biopsies. At least six samples should be taken from different parts of the colon, because inflammation can be patchy. Missing even one biopsy can mean missing the diagnosis.
Studies show that when biopsies are done properly, microscopic colitis is found in up to 15% of patients with unexplained chronic diarrhea. That’s not rare. It’s underdiagnosed.
Budesonide: The Gold Standard Treatment
Once diagnosed, the first-line treatment isn’t antibiotics, fiber supplements, or herbal remedies. It’s budesonide. This isn’t your grandparent’s steroid. Unlike prednisone, which floods your whole body with hormones, budesonide is designed to act almost entirely in the gut.
How? It’s metabolized by the liver before it can enter the bloodstream. About 90% of it gets broken down on the first pass-meaning only 10 to 15% actually circulates systemically. That’s why side effects like weight gain, high blood sugar, or bone loss are rare compared to traditional steroids.
Multiple clinical trials confirm its effectiveness. In the MICRO-1 and MICRO-2 studies, 84% of patients with collagenous colitis went into complete remission after 8 weeks of 9 mg daily budesonide. Placebo? Only 38%. For lymphocytic colitis, the numbers are similar: 75 to 85% response rate versus 25 to 30% with dummy pills.
Most patients feel better within 2 weeks. One patient on Reddit wrote: “Went from 10 bathroom trips a day to 2 in 10 days. I cried the first morning I didn’t need to plan my day around a toilet.” That’s not hype-that’s the data.

How It’s Used: Dosing and Duration
The standard starting dose is 9 mg per day, taken as a capsule, for 6 to 8 weeks. That’s enough to calm the inflammation in most people. After that, doctors typically stop the drug to see if symptoms stay away.
But here’s the catch: relapse is common. Between 50 and 75% of people see symptoms return after stopping budesonide. That doesn’t mean it didn’t work-it means the disease is still there, just quiet.
For those who relapse, maintenance therapy is often needed. A lower dose-6 mg daily or even 3 mg every other day-can keep symptoms under control for months or years. Some patients stay on it for over a year. Long-term safety data beyond 12 months is still limited, but current evidence suggests the risk remains low, especially compared to the toll of ongoing diarrhea.
Doctors recommend tapering slowly: reduce by 3 mg every 2 to 4 weeks. Jumping off cold turkey increases relapse risk. And if symptoms come back during tapering, it’s not failure-it’s a signal to adjust the plan.
Other Treatments-And Why They Fall Short
There are alternatives, but none match budesonide’s balance of power and safety.
- Bismuth subsalicylate (Pepto-Bismol): Works for some-about 26% remission-but you’d need to take 4 to 6 tablets a day, which can cause black stools and, rarely, ringing in the ears.
- Mesalamine: Used in ulcerative colitis, but only helps 40 to 50% of MC patients. Not strong enough for moderate-to-severe cases.
- Cholestyramine: Good if bile acid malabsorption is the trigger (which it is in many MC cases). Works in 60 to 70% of those patients, but it’s a powder you mix with water-taste is awful, and it interferes with other meds.
- Prednisone: Works just as well as budesonide, but causes insomnia, mood swings, high blood sugar, and bone thinning in nearly half of users. Not worth the trade-off.
- Biologics like infliximab: Reserved for extreme cases. Costs $2,500 to $3,000 per infusion. Only 20 to 30% respond. Risk of serious infections. Too heavy for routine use.
Budesonide isn’t perfect, but it’s the best tool we have right now. It’s the only treatment with strong, high-quality evidence behind it. European and North American guidelines agree: start with budesonide.
Real-World Experience: What Patients Say
On patient forums like PatientsLikeMe and Reddit, feedback is mixed but mostly positive. Of 247 users surveyed, 68% reported major improvement within two weeks. Many praised the speed of relief and the lack of severe side effects.
But 32% had negative experiences. The most common complaints:
- Insomnia (15%)
- Acne or skin changes (12%)
- Mood swings or anxiety (8%)
- High cost without insurance ($800-$1,200 for branded Entocort EC)
- Relapse after stopping (65%)
One patient wrote: “Worked great for 6 weeks. Then symptoms came back. Now I’m on maintenance for two years. I don’t want to be on steroids forever, but I don’t want to go back to the bathroom every hour either.”
Some find success combining treatments. “Budesonide plus cholestyramine fixed me after three years,” said another. That’s not in the guidelines-but it works for some.
Cost, Access, and the Future
Since 2018, generic budesonide has been available, cutting the price by 60%. A full 8-week course now costs $150 to $250 without insurance. That’s manageable for most. The branded version, Entocort EC, is still sold-but rarely necessary.
Still, cost isn’t the only barrier. Many doctors still don’t know to test for MC. Patients have to advocate for themselves. Ask for biopsies if you have chronic watery diarrhea. Don’t settle for “it’s just IBS.”
The future is looking brighter. In 2023, the FDA gave Fast Track status to vedolizumab, a biologic that targets gut-specific inflammation. Early results show 65% remission in refractory cases. The European Microscopic Colitis Group is also exploring fecal calprotectin as a non-invasive way to monitor treatment-no more repeat colonoscopies.
And research is now looking at genetics. Early data suggests people with HLA-DQ2 or HLA-DQ8 genes respond better to budesonide. That could mean personalized treatment down the line: test your DNA, then pick your drug.
What You Should Do Next
If you’ve had unexplained diarrhea for more than a month:
- Stop assuming it’s IBS or food sensitivity.
- Ask your doctor for a colonoscopy with multiple biopsies-at least six, from different areas.
- If MC is confirmed, discuss starting budesonide 9 mg daily for 6-8 weeks.
- Monitor for side effects: insomnia, mood changes, acne. These are usually mild and temporary.
- If symptoms return after stopping, don’t give up. Maintenance dosing is a valid option.
- Consider adding cholestyramine if you have bile acid issues-ask your doctor for a trial.
Microscopic colitis isn’t life-threatening, but it’s life-disrupting. The good news? You don’t have to live with it. With the right test and the right treatment, you can get your life back.
Can microscopic colitis be cured?
There’s no permanent cure yet, but most people achieve long-term symptom control. About 25 to 40% of patients go into sustained remission after a single course of budesonide. For others, maintenance therapy or combination treatments keep symptoms under control for years. Some cases resolve on their own after 2 to 3 years, but that’s unpredictable.
Is budesonide safe for long-term use?
For most people, yes. Because budesonide is mostly broken down by the liver, systemic exposure is low. Studies show minimal impact on bone density, blood sugar, or adrenal function in patients on maintenance doses for up to 2 years. However, long-term use beyond 24 months isn’t well studied. Doctors monitor blood pressure, HbA1c, and bone density in older patients as a precaution.
Can I take budesonide if I have liver disease?
No-not if you have severe liver disease (Child-Pugh Class C). Budesonide relies on liver metabolism to limit side effects. If your liver can’t process it, you’ll get higher levels in your blood, increasing the risk of steroid side effects. Mild or moderate liver disease may be okay with close monitoring, but always consult your doctor.
Why do I need a biopsy if my colonoscopy looks normal?
Because microscopic colitis doesn’t cause visible changes. The inflammation is only visible at the cellular level. A normal colonoscopy doesn’t rule it out-it’s why the condition is so often missed. Biopsies are the only way to confirm the diagnosis. At least six samples should be taken from different parts of the colon to avoid false negatives.
How do I know if budesonide is working?
You’ll notice symptom changes within 7 to 14 days. Fewer bowel movements, less urgency, no more nighttime trips. If you’re going from 8 to 10 stools a day down to 1 or 2, that’s a clear sign. If you don’t see improvement after 4 weeks, talk to your doctor. You might need a higher dose, a longer course, or a different approach.
Are there natural remedies that work for microscopic colitis?
No proven natural remedies exist. Diets like low-FODMAP or gluten-free may help a subset of patients, especially if there’s a food trigger, but they don’t treat the underlying inflammation. Probiotics, turmeric, or peppermint oil may ease general discomfort, but they won’t induce remission. Budesonide remains the only treatment with strong clinical evidence for stopping the disease process.
What happens if I stop budesonide too soon?
You’re likely to relapse. Studies show 50 to 75% of patients return to symptoms within 6 months of stopping abruptly. Tapering slowly-reducing by 3 mg every 2 to 4 weeks-lowers relapse risk. If symptoms come back during tapering, it’s not a failure. It means your body still needs anti-inflammatory support. Maintenance therapy is a legitimate, common next step.
Microscopic colitis is real. It’s common. And it’s treatable. You don’t have to keep living with constant diarrhea. Ask for the right test. Start the right treatment. And don’t let a normal colonoscopy fool you-sometimes, the truth is only visible under a microscope.
Alyssa Torres
November 20, 2025 AT 14:56I was diagnosed with collagenous colitis last year after 14 months of being told it was IBS. I cried when my doctor finally ordered biopsies. I went from 10+ trips a day to 2 after 3 weeks on budesonide. I’m now on 3mg every other day as maintenance and honestly? I’d take that over the chaos any day. You’re not weak for needing it-you’re smart for finding it.
Summer Joy
November 20, 2025 AT 19:52OMG I’m so done with doctors who think diarrhea = stress 😭 I had to beg for 8 biopsies and they still missed it on the first go. Then I got the diagnosis and was like ‘wait… I’ve been suffering for 3 years because NO ONE LOOKS CLOSE ENOUGH?’ Budesonide saved me but also made me break out like a teen. Worth it? YES. But also… why is this not standard testing??
Aruna Urban Planner
November 22, 2025 AT 01:00The pharmacokinetics of budesonide are elegantly designed-first-pass hepatic metabolism minimizes systemic exposure while maximizing local anti-inflammatory effects in the colon. This targeted delivery profile distinguishes it from classical corticosteroids, which lack tissue specificity. The clinical efficacy data from MICRO-1/2 is robust, with remission rates exceeding 80% in collagenous colitis. However, the high relapse rate post-tapering suggests persistent subclinical inflammation, implying MC may be a chronic immune dysregulation rather than an acute, self-limiting entity.
Nicole Ziegler
November 23, 2025 AT 05:08me too. budesonide = my new bestie 🙌 no more panic attacks before leaving the house. also, the generic is like $180 now?? game changer. i just wish my doc had known sooner 😔
Bharat Alasandi
November 24, 2025 AT 19:06bro i had this for 5 years. doc said ‘drink more water’. i was like bro i’m pooping 12x a day. finally found a gastro who knew what biopsies were. budesonide worked like magic. now i’m on 3mg every 3 days and life’s back. no more panic buying toilet paper before road trips 😅
Kristi Bennardo
November 26, 2025 AT 12:51This is dangerous medical advocacy. Budesonide is a steroid. You are normalizing long-term steroid use in a population already vulnerable to osteoporosis and metabolic dysfunction. The FDA has not approved it for maintenance therapy. This post is irresponsible. Patients need to be warned about systemic effects-even low-dose steroids accumulate over time. This is not ‘safe’-it’s pharmacologically risky.
Shiv Karan Singh
November 28, 2025 AT 02:50lol budesonide? yeah right. you all know the pharma companies paid the ‘studies’ to make it look good. i’ve seen 3 people on it get adrenal crash after stopping. and the ‘68% improvement’? probably just placebo. i bet 80% of these people just went gluten-free and called it a day. also, why is everyone ignoring the fact that MC might be linked to glyphosate? anyone else think about that?
Ravi boy
November 28, 2025 AT 08:34my mom had this and took budesonide for 2 years. she said the worst part was the insomnia but she’d take it again. i asked her if she ever tried turmeric and she said ‘baby i tried everything before this’ lol. biopsies are key. my doc almost skipped them. dont let them skip em
Matthew Karrs
November 28, 2025 AT 23:31why is no one talking about the fact that the ‘84% remission’ stat comes from a trial funded by the manufacturer? and the ‘long-term safety’? they’ve only studied it for 2 years. what about 10? 20? and why are they pushing this instead of researching the real cause? this feels like a distraction from bigger pharma lies. i’m not taking it.
Matthew Peters
November 29, 2025 AT 09:09Just wanted to say thank you to everyone who posted here. I’m 58 and had this for 2 years. I thought I was losing my mind. I asked for biopsies on my third colonoscopy and got diagnosed. Started budesonide and within 10 days I slept through the night for the first time in years. I’m on maintenance now. I don’t know if I’ll ever be ‘cured’ but I’m not living in fear anymore. This isn’t just a medical post-it’s a lifeline.