Statin Muscle Symptoms Assessment
Is your muscle pain likely statin myopathy or neuropathy?
This tool helps you distinguish between two common statin side effects: myopathy (muscle damage) and neuropathy (nerve damage). Your answers will help determine which condition is most likely causing your symptoms.
Millions of people take statins to lower cholesterol and protect their hearts. But if you’ve started feeling strange muscle cramps, aching, or tingling in your legs, it’s natural to wonder: is this the statin? And more importantly - is it your muscles or your nerves?
Statin Muscle Cramps Are Common - But Not Always What They Seem
About 7 to 29% of people on statins report muscle discomfort. That’s a lot. But here’s the catch: most of these cases aren’t dangerous. Many are mild, temporary, or even unrelated to the drug. The real problem? Doctors and patients often mix up two very different problems: statin-associated myopathy and statin-related neuropathy.Myopathy means muscle damage. Neuropathy means nerve damage. They feel similar - both can cause cramps, weakness, or pain - but they need totally different responses. Mistake one for the other, and you could stop a life-saving medication unnecessarily… or keep taking it when you shouldn’t.
What Statin Myopathy Actually Looks Like
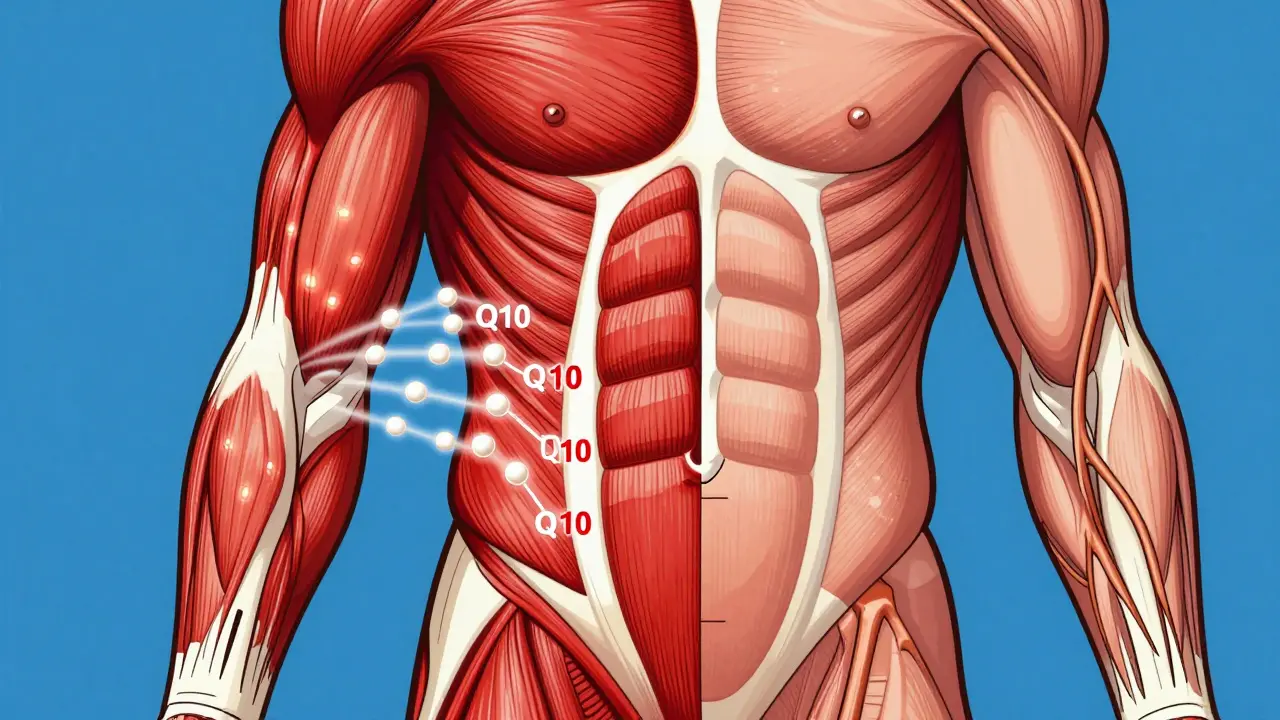
Statin myopathy is muscle pain or weakness that shows up because the drug interferes with how your muscles make energy. Statins block HMG-CoA reductase - a key enzyme in cholesterol production. But that same enzyme is also needed to make coenzyme Q10, which your muscles use to generate power. When CoQ10 drops by 40% within weeks of starting a statin, your muscles start to struggle.The classic signs of myopathy:
- Deep, dull aches in your thighs, hips, or shoulders - not sharp or shooting
- Bilateral symptoms (both sides, not just one leg)
- Weakness when climbing stairs, rising from a chair, or lifting your arms
- No numbness, tingling, or burning
- CK levels may be normal or slightly elevated (but not always)
What’s tricky? Many people don’t realize they’re weaker. They just think they’re getting older. You might notice you’re slower walking, need to use your arms to push up from the couch, or avoid hills. That’s not normal aging - that’s muscle fatigue from statins.
True myopathy with CK levels more than 4 times the upper limit is rare - about 1 in 10,000 people per year. But mild, subclinical myopathy is far more common. And if you’re over 65, female, taking a fibrate like fenofibrate, or have the HLA-DRB1*11:01 gene variant, your risk goes up.
Neuropathy? The Confusing, Controversial Link
Now, what about tingling, burning feet, or numbness in your hands? That’s classic neuropathy. Some people assume statins cause this too. But the science is messy.Here’s what we know: nerves need cholesterol to stay healthy. They use it to build their protective sheaths. Statins lower LDL - and LDL carries vitamin E, an antioxidant that protects nerves. So theoretically, statins could hurt nerves by starving them of cholesterol and vitamin E.
But here’s the twist: a 2019 study of over 600 people with unexplained nerve damage found that those taking statins were less likely to have neuropathy. Their odds were cut in half. Other studies show no link at all. The NIH calls statin-induced neuropathy “probable,” not confirmed.
So if you have burning toes or pins-and-needles in your fingers, it’s far more likely to be:
- Diabetes (the #1 cause)
- Vitamin B12 deficiency
- Alcohol use
- Spinal stenosis
- Autoimmune nerve disease
Statin-related neuropathy, if it exists at all, is rare. And it’s not the same as myopathy. Neuropathy affects sensation - not strength. You won’t drop things because your muscles are weak. You’ll drop things because you can’t feel them.

How to Tell Them Apart - The Real Diagnostic Clues
You can’t rely on symptoms alone. You need to look at the full picture. Here’s how to spot the difference:| Feature | Statin Myopathy | Neuropathy (Any Cause) |
|---|---|---|
| Location | Proximal muscles: thighs, hips, shoulders | Distal limbs: feet, hands - stocking-glove pattern |
| Primary Symptom | Weakness, aching, fatigue | Numbness, tingling, burning, electric shocks |
| CK Levels | Normal or elevated (often >4x ULN in true cases) | Always normal |
| Nerve Tests | Normal nerve conduction | Reduced sensory nerve signals |
| Response to Stopping Statin | Improves within weeks to months | No change - symptoms persist or worsen |
| Common Triggers | High-dose statins, age >65, fibrate combo, genetics | Diabetes, B12 deficiency, alcohol, spinal issues |
If your cramps are in your thighs and you struggle to stand up, get your CK checked. If your toes feel like they’re wrapped in plastic and you can’t tell if your socks are on, get a nerve test. Don’t guess.
What to Do If You’re Having Muscle Cramps on Statins
Don’t quit your statin on your own. That’s dangerous. Cardiovascular risk drops 25% for every 1 mmol/L drop in LDL. Stopping without a plan increases your chance of heart attack or stroke.Here’s what your doctor should do:
- Check your CK levels - if normal, myopathy is unlikely
- Test for thyroid disease, vitamin D, and B12 - these mimic muscle weakness
- Review all other meds - especially fibrates, cyclosporine, or certain antibiotics
- If symptoms point to myopathy: try switching to a different statin
- If symptoms point to neuropathy: rule out diabetes, B12, alcohol - don’t assume it’s the statin
Switching statins works in about 60% of cases. Hydrophilic statins like pravastatin or rosuvastatin are less likely to cause muscle issues than lipophilic ones like simvastatin or atorvastatin. If you had a bad reaction to one, try another - but do it under supervision.
CoQ10 supplements? A 2015 JAMA trial of 44 patients showed no benefit over placebo. Don’t waste money. Genetic testing for SLCO1B1 (which increases simvastatin risk 4.5-fold) can help if you’ve had repeated problems.
When to See a Neurologist
If your symptoms don’t improve within 2 to 3 months after stopping the statin, you need a neurologist. That’s the rule from the Cleveland Clinic. Why? Because sometimes, the statin was hiding something else.Imagine this: you’ve had mild nerve damage from undiagnosed diabetes for years. The statin made your muscles ache, so you stopped it. Now the muscle pain is gone - but the numbness in your feet is still there. Was it the statin? Or was the statin masking the real problem?
That’s why you need nerve conduction studies. They show if your nerves are damaged, and if so, how badly. Without them, you’re flying blind.
The Bottom Line: Don’t Stop - Figure It Out
Statin muscle cramps are common. But they’re not always the statin’s fault. And when they are, it’s usually myopathy - not neuropathy. The good news? You don’t have to live with it. You don’t have to give up your heart protection.Work with your doctor. Get the right tests. Switch statins if needed. Add ezetimibe or a PCSK9 inhibitor if you’re truly intolerant. Millions of people manage statin side effects and still live long, healthy lives. You can too.
Just don’t assume. Don’t guess. Test. Diagnose. Act.
Can statins cause muscle cramps in the calves?
Yes, but it’s less common. Statin myopathy usually affects proximal muscles like thighs and hips first. Cramps in the calves can happen, especially if weakness spreads. But if the cramps are isolated to the calves with no weakness elsewhere, it’s more likely due to dehydration, electrolyte imbalance, or overuse - not statins.
Should I take CoQ10 with my statin to prevent cramps?
Not based on current evidence. A large 2015 JAMA study found CoQ10 supplements didn’t reduce muscle symptoms in statin users any better than placebo. While the theory makes sense - statins lower CoQ10, and muscles need it - the clinical benefit hasn’t been proven. Save your money unless your doctor recommends it for another reason.
Is statin-induced neuropathy real?
It’s possible, but not proven. Some studies suggest a link, but others - including a well-designed 2019 case-control study - found statins might actually lower neuropathy risk. Most experts agree: if you have nerve symptoms, look for diabetes, B12 deficiency, or alcohol first. Don’t blame the statin unless all other causes are ruled out.
How long does it take for statin muscle pain to go away after stopping?
Most people notice improvement within 2 to 6 weeks. Full recovery can take 3 to 6 months, especially if the muscle damage was mild but long-standing. If pain persists beyond 3 months after stopping, see a neurologist - you may have an unrelated condition that was masked by the statin.
Can I restart a statin after having muscle cramps?
Yes, in most cases. About 60% of people who had muscle symptoms can tolerate a different statin - especially hydrophilic ones like pravastatin or rosuvastatin. Start low, go slow, and monitor closely. Never restart without medical supervision. Some people need non-statin options like ezetimibe or PCSK9 inhibitors instead.
Next Steps: What to Do Today
- If you’re on a statin and have new muscle pain: write down when it started, where it hurts, and what makes it worse or better.
- Call your doctor. Ask for a CK blood test - it’s simple and cheap.
- If you have tingling or numbness: ask about checking your blood sugar and B12 levels.
- Don’t stop your statin until you’ve talked to your doctor. Heart risk doesn’t wait.
- If you’ve been told your cramps are “just aging” - push back. Muscle weakness isn’t normal at any age.
You’re not imagining this. You’re not overreacting. You’re just someone trying to stay healthy - and you deserve answers that make sense.
Josh josh
January 25, 2026 AT 06:35statins are just big pharma’s way of making us pay for normal aging bruh
Renia Pyles
January 26, 2026 AT 23:06Oh so now it’s not the statin but your diabetes? Yeah right. I’ve been on simvastatin for 8 years and my feet feel like they’re stuffed in wet socks. Your ‘science’ is just corporate spin. I don’t care what some 2019 study says-I feel it. And I’m not alone.
Dan Nichols
January 27, 2026 AT 09:40Let me guess you’re the type who thinks muscle cramps are ‘just aging’ until you can’t get off the couch. The CK levels don’t lie. If your creatine kinase is normal and you’re still cramping, it’s not myopathy. You’re either dehydrated or you’ve been sitting too long watching Netflix. Stop blaming pills and start blaming your lifestyle.
Ashley Karanja
January 28, 2026 AT 04:45What’s fascinating here is the epistemological tension between phenomenological experience and biochemical reductionism. On one hand, we have the lived reality of patients reporting sensory disturbances-burning, tingling, electric shocks-that align with peripheral neuropathy. On the other, population-level studies suggest no causal link, or even a protective effect, possibly mediated by cholesterol’s role in myelin integrity and vitamin E transport. This isn’t just a pharmacological question-it’s a hermeneutic one. How do we validate subjective suffering when objective biomarkers are inconclusive? The answer may lie not in binaries (statin = good/bad) but in personalized biopsychosocial mapping. Maybe the statin isn’t the villain-it’s the canary in the coal mine, revealing an underlying metabolic vulnerability we’ve ignored for decades.
bella nash
January 28, 2026 AT 14:51It is imperative to underscore that the cessation of statin therapy without medical supervision constitutes a potentially life-threatening deviation from evidence-based clinical guidelines. The statistical reduction in cardiovascular mortality is not merely significant-it is unequivocal. To conflate transient muscular discomfort with irreversible neurological pathology is not only scientifically unsound but ethically precarious.
Allie Lehto
January 30, 2026 AT 07:13everyone says 'don't stop your statin' but no one tells you what to do when your legs feel like they're full of sand and your feet are on fire. i stopped mine after 3 months and the cramps went away... but then my cholesterol went up 40 points. so now i'm stuck between a heart attack and a neurological nightmare. thanks for the advice doc. 😔
Henry Jenkins
January 30, 2026 AT 21:41I’ve been on rosuvastatin for 5 years and had zero issues until last winter. Then I started getting this deep, dull ache in my hips-nothing sharp, just constant fatigue like I’d run a marathon in my sleep. I got my CK checked, it was normal. Then I asked for a B12 test. My level was 180. I started injections. Within 3 weeks, the weakness was gone. No statin change needed. The point is: we’re too quick to blame the drug. Maybe the real problem is hidden in plain sight. Check your vitamins. Check your thyroid. Check your sugar. Don’t just assume it’s the statin. And if you’re over 60? Get a nerve conduction test before you panic. It’s not expensive, and it saves you from ditching a lifesaver.
TONY ADAMS
February 1, 2026 AT 01:08my grandma took statins and her legs started shaking like she had the shakes. she said it felt like bugs crawling under her skin. doc said it was anxiety. she died of a heart attack 6 months later. i’m not taking any chances. i’m off statins. period.
Shweta Deshpande
February 1, 2026 AT 07:16Thank you for writing this so clearly! I’ve been telling my friends for years that muscle pain on statins doesn’t always mean it’s the drug-sometimes it’s just low vitamin D or B12. I had the same tingling in my toes and thought it was the statin. Turned out I was borderline diabetic. Now I’m on metformin and my feet feel normal again. Don’t panic-test first! And yes, CoQ10 is a waste of money unless your doctor says otherwise. You’re not alone, and you’re not crazy. Just get checked. 💪❤️