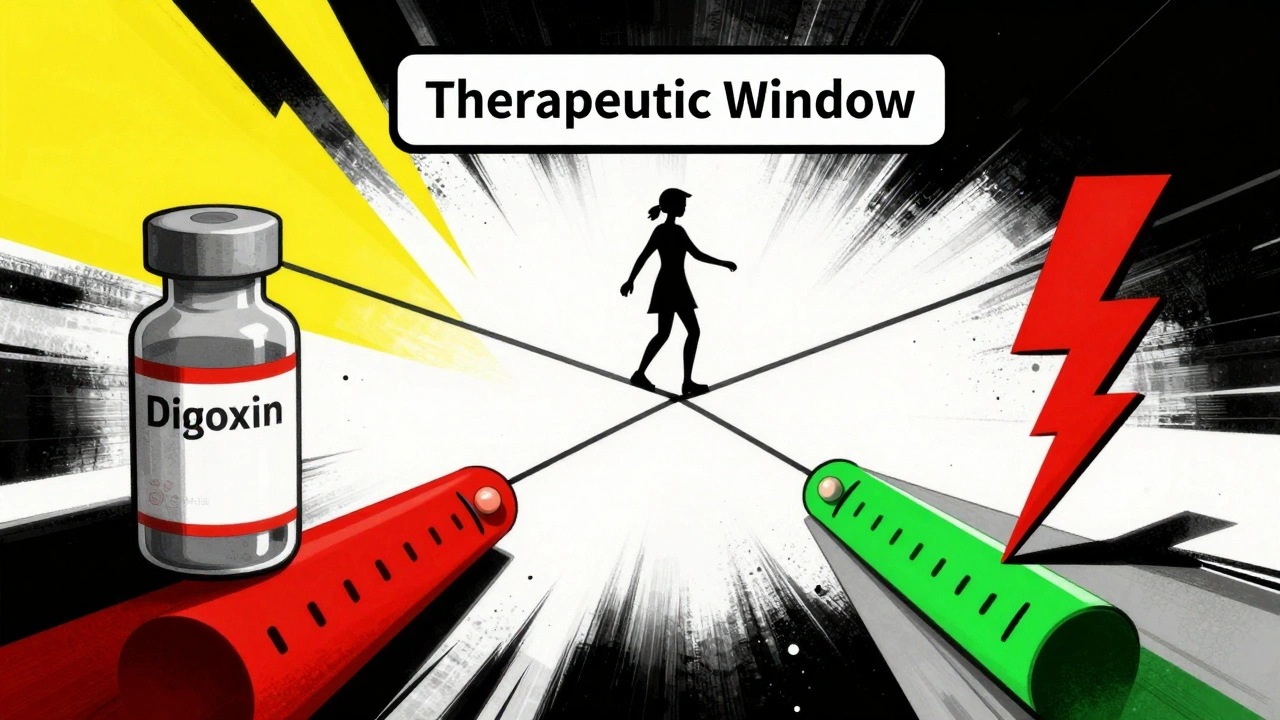
Some medications are like walking a tightrope. Take just a little more, and you risk serious harm. Take a little less, and the treatment doesn’t work. These are NTI drugs - Narrow Therapeutic Index medications. They don’t have room for error. A 10% change in dose can send a patient from safe to dangerous. And yet, millions rely on them every day.
What Makes a Drug an NTI Drug?
An NTI drug has a tiny gap between the dose that works and the dose that harms. The FDA defines it simply: small changes in blood levels can cause life-threatening side effects or make the drug useless. For most medicines, your body can handle some variation. Not with NTI drugs. Their therapeutic window is razor-thin.
Take digoxin, used for heart rhythm problems. The safe range? 0.5 to 2.0 nanograms per milliliter of blood. Go above 2.0? Risk of fatal heart arrhythmias. Drop below 0.5? The heart condition comes back. That’s a 4-fold window - barely enough space to breathe. Compare that to a common antibiotic like amoxicillin, where you could double or triple the dose without immediate danger.
This isn’t just theory. Studies show NTI drugs make up only about 15% of medications that need blood level monitoring, but they cause 30% of dosing-related hospitalizations. That’s why pharmacists and doctors treat them differently - with extra caution, extra checks, and extra communication.
The Core NTI Drug List You Need to Know
There’s no single official list from the FDA, but multiple trusted sources - state pharmacy boards, transplant centers, and clinical guidelines - agree on a core group. Here are the most common NTI drugs you’ll encounter in practice:
- Warfarin - The classic anticoagulant. Therapeutic range is measured by INR: 2.0 to 3.0 for most conditions. An INR over 4.0 raises bleeding risk by more than 7 times. Even small changes in diet, other meds, or genetics can throw it off.
- Digoxin - Used for heart failure and atrial fibrillation. As mentioned, the range is 0.5-2.0 ng/mL. Toxicity can cause nausea, confusion, and deadly heart rhythms.
- Lithium - A mood stabilizer for bipolar disorder. Safe level: 0.6 to 1.2 mmol/L. Above 1.5? Tremors, confusion, kidney damage. Below 0.5? Depression returns. Many patients need blood tests every 3-6 months.
- Phenytoin - An older but still used seizure medication. Therapeutic range: 10-20 mcg/mL. Too high? Slurred speech, dizziness, even coma. Too low? Seizures return. It interacts with dozens of other drugs, making dosing a puzzle.
- Carbamazepine - Another antiseizure drug, also used for nerve pain. Range: 4-12 mcg/mL. Its metabolism varies wildly between people due to genetics, so one person’s safe dose could be toxic to another.
- Tacrolimus - A key immunosuppressant after organ transplants. Target trough: 5-15 ng/mL. A level of 20? Kidney damage. A level of 3? Rejection risk skyrockets. Transplant patients get tested 3 times a week in the early weeks.
- Sirolimus - Also used after transplants. Same therapeutic range as tacrolimus: 5-15 ng/mL. Like tacrolimus, it’s highly sensitive to food, other drugs, and even the time of day it’s taken.
- Levothyroxine - The most common thyroid replacement. Not measured by blood concentration, but by TSH levels: 0.5-4.5 mIU/L. A tiny change in brand or generic can cause TSH to jump from 1.2 to 8.7 - meaning the patient becomes hypothyroid. Many patients report fatigue, weight gain, or depression after switching generics.
Why Generic Substitutions Can Be Dangerous
For most drugs, switching from brand to generic is safe and saves money. Not with NTI drugs. The FDA requires stricter bioequivalence standards for these - 90% to 111% similarity in blood levels, instead of the usual 80% to 125%. But even that isn’t foolproof.
A 2023 Reddit thread from a pharmacist detailed a case: a 62-year-old woman switched from one brand of levothyroxine to a generic. Her TSH jumped from 1.2 to 8.7. She was told it was "just a fluke." It wasn’t. It took three months of testing and dose tweaks to get her back to normal. She had gained 15 pounds, felt exhausted, and her heart rate dropped dangerously low.
Forty-seven U.S. states have laws restricting automatic substitution of NTI drugs. Twenty-eight require the doctor to write "dispense as written" or "no substitution" on the prescription. Yet, many patients still get switched without knowing - and end up in the ER.
Monitoring: The Lifeline for NTI Drugs
There’s no way around it: if you’re on an NTI drug, you need regular blood tests. No exceptions.
- Warfarin: INR checked every 3-5 days when starting, then weekly until stable.
- Lithium: Blood levels every 3-6 months, more often if kidney function changes or you’re elderly.
- Phenytoin and carbamazepine: Trough levels checked every 2-4 weeks initially, then every 3-6 months.
- Tacrolimus and sirolimus: Trough levels 3 times a week in the first month after transplant, then weekly, then monthly.
- Levothyroxine: TSH checked 6-8 weeks after any dose change or brand switch.
These tests aren’t optional. A 2022 study found 32% of lithium patients missed their monitoring appointments. Many didn’t realize how dangerous skipping a test could be. One patient ended up in the hospital with lithium toxicity after going 11 months without a check-up.
Cost is a barrier. Each test runs $25-$150. Medicare covers 80%, but patients still pay out-of-pocket. Many skip tests because of cost or inconvenience - and pay the price later.
Emerging NTI Drugs: The New Frontier
The list isn’t static. Newer cancer drugs are joining it. Targeted therapies like axitinib (for kidney cancer), ponatinib (for leukemia), and olaparib (for ovarian cancer) have therapeutic ranges measured in single-digit nanograms per milliliter. Their effectiveness depends on precise dosing - and their side effects can be severe if levels creep up.
The FDA is now reviewing whether newer anticoagulants like apixaban and rivaroxaban should be added to the NTI list. While they’re safer than warfarin overall, bleeding risks still spike at higher doses. The European Medicines Agency says they’re not NTI. The Institute for Safe Medication Practices disagrees. The debate continues - and patients are caught in the middle.
What Patients Should Do
If you’re on one of these drugs, here’s what you need to do:
- Know your drug’s name and why it’s classified as NTI.
- Ask your doctor: "What’s my target level? What happens if it goes too high or too low?" Write it down.
- Never switch brands or generics without talking to your doctor. Even if the pharmacy says it’s "the same."
- Keep a log: record your doses, any side effects, and when you had your last blood test.
- Ask your pharmacist: "Is this the same brand I was on before?" If they say yes, double-check the label.
Don’t assume your doctor knows everything. Many physicians aren’t trained in therapeutic drug monitoring. Pharmacists are. Talk to both.
The Bigger Picture
NTI drugs are a growing part of modern medicine. As treatments get more precise - especially in cancer and transplant care - more drugs will fall into this category. The global market for NTI drugs is expected to hit $72 billion by 2028.
But the real challenge isn’t science. It’s systems. Only 45% of hospital electronic records have alerts when NTI drug levels go out of range. Many clinics still rely on paper logs. Patients get lost in the gaps.
There’s hope. The NIH is funding research on using genetics to personalize NTI dosing. Early results show a 40% faster path to safe levels for patients on warfarin and phenytoin. Wearable sensors that track drug levels in real time are in development.
Until then, the safest approach is simple: know your drug, stick to your schedule, and never skip a test. Because with NTI drugs, there’s no room for guesswork.
Stacy Tolbert
December 9, 2025 AT 08:58I had a friend on lithium who switched generics and ended up in the ER. She didn’t even know it was an NTI drug until her hands were shaking and she couldn’t remember her own birthday. Pharmacies don’t warn you. Doctors don’t explain. It’s terrifying how easy it is to get poisoned by accident.
Katherine Rodgers
December 10, 2025 AT 10:47so like… ntis are just drugs that make pharmacists rich? lol. 3x a week blood tests? for a pill? my dog gets more attention than my med schedule. also why is levothyroxine on here? its literally just a hormone. like… why not add water? you can overdose on that too.
Guylaine Lapointe
December 11, 2025 AT 16:59This post is dangerously incomplete. You mention the FDA’s 90–111% bioequivalence standard for NTI drugs, but you fail to acknowledge that even within that range, individual pharmacokinetic variability can cause clinically significant deviations. The FDA’s standards are a legal fiction designed to appease generic manufacturers-not a guarantee of safety. And yet, 78% of patients are never informed of this risk. This isn’t medical care. It’s corporate negligence dressed up as efficiency.
Suzanne Johnston
December 11, 2025 AT 19:13People treat NTI drugs like they’re magic bullets, but the real issue is systemic. We don’t have enough pharmacists. We don’t train doctors on TDM. We don’t fund monitoring. And then we blame patients for missing appointments. We’ve built a system where people have to be experts just to stay alive. That’s not healthcare. That’s a survival game with no instruction manual.
Graham Abbas
December 13, 2025 AT 05:46Every time I see someone say "it’s just a pill," I want to scream. These aren’t vitamins. They’re precision instruments. Imagine driving a Ferrari with no speedometer, no brake pedal feedback, and the manufacturer saying "it’s fine, just guess." That’s what it’s like being on warfarin or tacrolimus. And yet, we act like it’s normal. It’s not normal. It’s a tragedy waiting to happen.
Haley P Law
December 15, 2025 AT 04:56my cousin just got switched to a new levothyroxine brand and now she’s crying in the shower every day 😭 her hair is falling out and she gained 20 lbs in 2 months. she called her doctor and they said "maybe try a different time of day?" like… are you kidding me??
Steve Sullivan
December 17, 2025 AT 01:31the fact that we let pharmacies swap ntis without consent is insane. i work in a clinic and we’ve had 3 patients this year alone crash into the hospital because some tech clicked "substitute" without telling anyone. one guy’s tacrolimus level went from 8 to 22 in 48 hours. he almost lost his kidney. the pharmacy said "it’s the same thing." no it’s not. it’s like swapping your car’s engine for a "similar" one and saying "it’ll run fine." also… why does no one talk about how expensive these tests are? $150 every month? for a person on fixed income? that’s a rent payment. we’re killing people with bureaucracy.
George Taylor
December 18, 2025 AT 01:53Why is this even a conversation? The answer is obvious: pharmaceutical companies profit from complexity. NTI drugs require monitoring. Monitoring requires labs. Labs require billing codes. Billing codes require paperwork. Paperwork requires staff. Staff requires salaries. Salaries require insurance billing. Insurance billing requires… you get it. The system is designed to make you dependent. And the worst part? You’re supposed to be grateful for the "care."
Chris Marel
December 18, 2025 AT 17:31This is eye-opening. In Nigeria, most people can’t even access basic meds, let alone regular blood tests. But I’ve seen patients on phenytoin in Lagos who get tested once a year-if they’re lucky. I wonder how many are suffering in silence because they don’t know what’s wrong. Maybe this list should be shared globally. Not just in the US.
William Umstattd
December 19, 2025 AT 13:58Let me be clear: allowing generic substitution of NTI drugs without explicit physician authorization is a crime. It’s not negligence. It’s not oversight. It’s a deliberate choice made by pharmacy chains and insurance companies to save pennies while risking lives. And those who defend it are complicit. If your pharmacy switches your levothyroxine without your consent, report them. Demand accountability. This isn’t medicine-it’s gambling with human lives.
Maria Elisha
December 21, 2025 AT 03:22so like… i just got prescribed carbamazepine and my doc said "take one pill" and that’s it. no talk about blood tests or anything. should i be worried??
Shubham Mathur
December 23, 2025 AT 00:39My uncle was on tacrolimus after his transplant. He got switched to a generic because his insurance said "no coverage" for the brand. Three weeks later he had acute kidney injury. They said it was "likely unrelated." It wasn’t. He spent 6 weeks in ICU. Now he’s on dialysis. Don’t let your insurance gamble with your organs. Fight back. Always ask: "Is this the exact same drug I was on?" If they say yes, ask for the manufacturer name. Write it down. And never trust a pharmacist’s word without proof.
Ruth Witte
December 23, 2025 AT 23:51THIS. THIS. THIS. 🙌 I’m on warfarin and I keep a spreadsheet of my INR, diet, meds, and even my sleep. My pharmacist calls me "the spreadsheet queen." But seriously-knowing your numbers saves your life. If you’re on an NTI drug, be your own advocate. Don’t wait for the system to catch up. Start tracking. Start asking. Start surviving.