Premedication Decision Tool
Do I Need Premedication?
This tool helps you determine if you need premedication based on your medical history.
Results will appear here
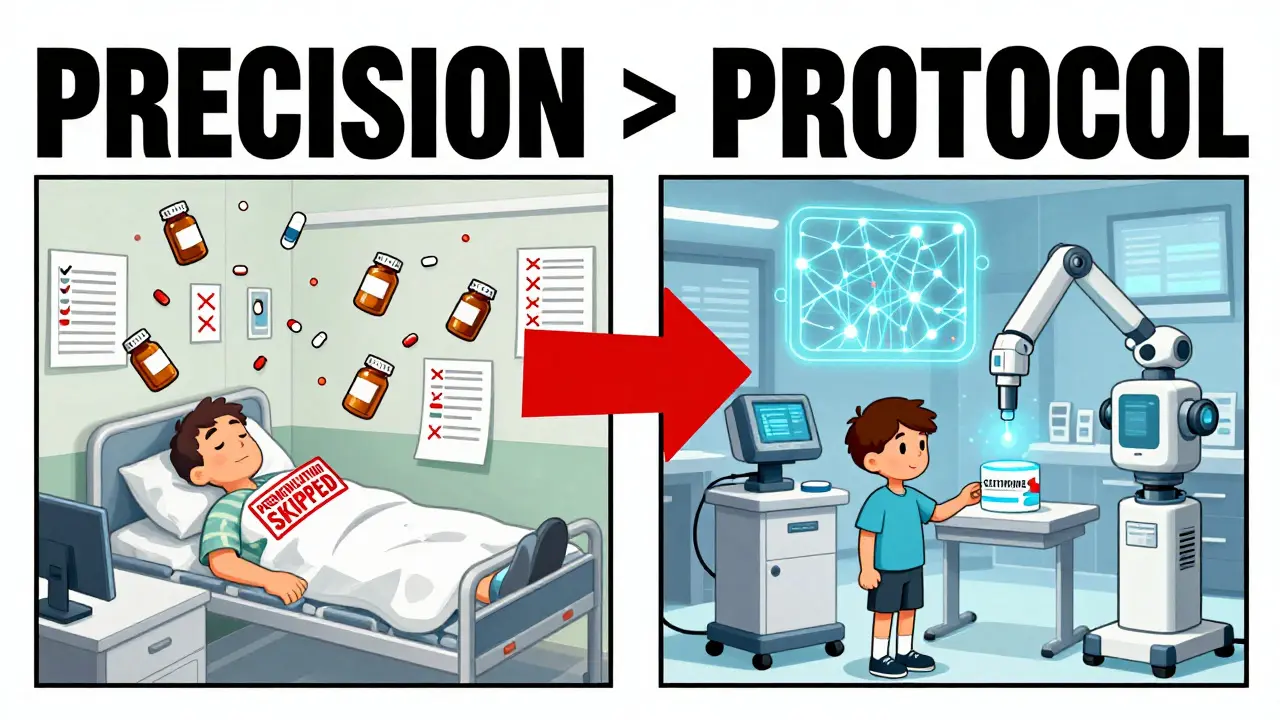
When you walk into a hospital for a CT scan or start chemotherapy, you’re not just getting a test or treatment-you’re stepping into a system designed to protect you from unseen dangers. One of the most effective, yet often misunderstood, layers of that protection is pre-medication. Specifically, the use of antiemetics, antihistamines, and steroids before procedures to prevent reactions that can turn routine care into a medical emergency.
It’s not about giving everyone a drug just in case. It’s about targeting the right people, with the right drugs, at the right time. And the data shows it works. In hospitals that follow modern protocols, moderate to severe reactions to contrast dye drop from nearly 1 in 200 patients to less than 1 in 2,500. That’s not luck. That’s science.
Why Pre-Medication Isn’t One-Size-Fits-All
For years, many clinics gave steroids and antihistamines to anyone getting contrast dye-even if they’d never had a reaction before. That changed. Now, guidelines from the American College of Radiology and Yale Medicine say: only give premedication to people who’ve had a prior reaction to the same type of contrast.
Why? Because these drugs aren’t harmless. Steroids can raise blood sugar. Antihistamines like diphenhydramine (Benadryl) can make you so sleepy you can’t drive home. Giving them to someone who doesn’t need them just adds risk without benefit.
The shift to targeted use is based on hard numbers. A 2022 study in Radiology found that 96% of moderate reactions were prevented in premedicated patients-but only 75% of severe ones. That means even with all the right drugs, you’re not 100% protected. So why give them to low-risk people? The answer: you don’t.
How the Drugs Work Together
Each of the three drug classes plays a different role.
- Steroids (like prednisone or methylprednisolone) calm down the immune system hours before the procedure. They don’t work fast. Oral prednisone needs at least 13 hours to hit full strength. IV methylprednisolone works faster-about 4 hours-but still needs planning.
- Antihistamines (cetirizine or diphenhydramine) block histamine, the chemical that triggers itching, hives, and flushing. Second-gen drugs like cetirizine (Zyrtec) are now preferred because they cause far less drowsiness. A 2021 JAMA Internal Medicine study showed 15.3% of patients on cetirizine felt sleepy versus 42.7% on diphenhydramine.
- Antiemetics (like ondansetron or aprepitant) are used mostly in chemotherapy, not imaging. They stop nausea and vomiting by blocking signals in the brain and gut. Triple therapy-ondansetron + aprepitant + dexamethasone-cuts CINV (chemotherapy-induced nausea and vomiting) from over 50% down to about 28%.
They’re not interchangeable. You can’t swap a steroid for an antiemetic. Each has its own target. Using them together is like putting on a seatbelt, airbag, and headrest-each one handles a different kind of impact.

Dosing by Age, Route, and Urgency
There’s no single dose that works for everyone. It changes based on whether you’re an adult, a child, or in an emergency.
For adults with prior contrast reactions:
- Outpatients: 50mg oral prednisone at 13, 7, and 1 hour before the scan, plus 10mg cetirizine within 1 hour of the injection.
- Inpatients or emergency: 40mg IV methylprednisolone 4 hours before, or 200mg IV hydrocortisone if methylprednisolone isn’t available. Antihistamine: 50mg IV diphenhydramine or 10mg oral cetirizine within 1 hour.
For children:
- Prednisone or prednisolone: 0.7mg per kg of body weight (max 50mg), given at the same intervals as adults.
- Over 6 months: cetirizine, based on weight (10mg for 30kg+).
- Under 6 months: diphenhydramine at 1mg/kg (max 50mg), because cetirizine isn’t approved for infants.
These aren’t guesses. They’re based on how the body absorbs and clears each drug. A child’s liver processes meds differently. An IV drug hits the bloodstream instantly. An oral pill takes time. Get this wrong, and you’re not protecting-you’re risking.
Where the System Breaks Down
Even with solid science, mistakes happen. A 2022 survey by the American Society of Health-System Pharmacists found that 68.3% of hospitals had errors in premedication orders. In 22.7% of those cases, the wrong drug or dose reached the patient.
Common issues:
- Scheduling nightmares: The 13-hour lead time for oral steroids means same-day referrals get turned away. A radiology tech in Toronto told Reddit’s r/radtech: “We’ve had zero severe reactions since we started Yale’s protocol-but we cancel 3-4 scans a week because the patient didn’t take their prednisone on time.”
- Documentation gaps: Nurses change shifts. Orders get lost. One patient got double the steroid dose because the old order wasn’t crossed out.
- Patient non-compliance: Oral meds are easy to forget. One study found 18% of outpatients skipped their premeds.
That’s why safety systems matter. Hospitals that use barcode scanning, EHR alerts, and standardized order sets cut errors by over 37%. Yale Medicine’s team spent 6 months working with pharmacy, nursing, and IT to build a system that auto-populates premed orders based on patient history. After a year, 94.7% of eligible patients got the right drugs on time.
What’s Changing Now
The field isn’t standing still. New tools are emerging.
First, infusion pumps with dose error-reduction systems are now required by the Institute for Safe Medication Practices (ISMP) for all IV premeds. These pumps won’t let you push more than the safe dose-even if the nurse types it in wrong.
Second, point-of-care barcode checks are being rolled out in surgical and radiology suites. Before you give the drug, you scan the patient’s wristband and the med. If they don’t match? The system stops you.
Third, AI is getting into the game. A 2023 study in the Journal of the American College of Radiology trained a machine learning model on 12,000 patient records. It predicted which patients would react to contrast with 83.7% accuracy-better than most human clinicians. That doesn’t mean we’ll stop using premeds. It means we’ll get smarter about who needs them.
And in oncology? The triple antiemetic combo (5-HT3 + NK1 + steroid) is now the gold standard. ASCO’s 2023 guidelines didn’t just confirm it-they made it mandatory for high-risk chemo like cisplatin. New drugs like fosnetupitant are coming, but they’re building on this foundation, not replacing it.
What Patients Should Know
If you’re scheduled for a scan or chemo:
- Ask: “Do I need premedication?” Don’t assume.
- If you’ve had a reaction before, bring details: what happened, when, and what drug you got.
- Ask about timing. If you’re told to take prednisone 13 hours before, set alarms. Skip it, and the protection doesn’t work.
- Know your antihistamine. Cetirizine (Zyrtec) is less sleepy. Diphenhydramine (Benadryl) might knock you out. Choose wisely.
- Report side effects. Even mild nausea or dizziness after a premed could mean something.
The goal isn’t to scare you. It’s to make sure you’re protected, not overmedicated. Pre-medication works. But only when it’s used right.
Do I need premedication if I’ve never had a reaction to contrast dye?
No. Current guidelines from the American College of Radiology and Yale Medicine recommend premedication only for patients with a documented prior reaction to the same type of contrast. Giving steroids or antihistamines to everyone increases risk without benefit. The goal is to protect those at real risk-not blanket-treat everyone.
Why is there a 13-hour wait for oral steroids?
Oral prednisone needs time to be absorbed, metabolized by the liver, and reach effective levels in the bloodstream. Studies show peak immune-suppressing effects occur 12-16 hours after ingestion. Giving it too late-like 2 hours before the scan-won’t help. That’s why protocols require doses at 13, 7, and 1 hour before: to maintain steady drug levels.
Is cetirizine better than diphenhydramine for premedication?
Yes, for most adults. Cetirizine (Zyrtec) is just as effective at preventing allergic reactions but causes far less drowsiness. A 2021 study in JAMA Internal Medicine found 15.3% of patients on cetirizine felt sleepy, compared to 42.7% on diphenhydramine. For patients who need to drive home or work after their scan, cetirizine is the clear choice. Diphenhydramine is still used in emergencies or for children under 6 months.
Can I skip my premedication if I’m feeling fine?
No. Even if you feel fine, your body may still be primed for a reaction. Premedication isn’t about treating symptoms-it’s about preventing them before they start. Skipping doses, even once, can remove your protection. One 2022 study showed that patients who missed their oral steroids had a 3x higher chance of a reaction than those who took all doses.
Are there alternatives to steroids for premedication?
Not yet. Steroids remain the only proven way to suppress the immune response that causes contrast reactions. While newer drugs like fosnetupitant are being tested for antiemetic use, no alternative has matched the effectiveness of corticosteroids for HSR prevention. Research is ongoing, but for now, steroids are still the standard.
