SEARCH
Depression: Understanding Causes, Treatments & Everyday Strategies
When dealing with depression, a mood disorder marked by persistent sadness, loss of interest, and low energy. Also known as major depressive disorder, it can affect anyone at any age. Recognizing the signs early helps you take action before it spirals. Below we’ll break down what drives depression, how it connects to other mental health issues, and what you can do right now.
Key Players in the Depression Landscape
One of the core tools doctors use is antidepressant medication, drugs that balance neurotransmitters like serotonin and norepinephrine to lift mood. These meds aren’t a magic fix, but they often provide the stability needed to start therapy or make lifestyle changes. Another powerful approach is cognitive behavioral therapy, a short‑term talk therapy that teaches you to spot and change negative thought patterns. When combined, medication and CBT create a two‑pronged attack: the meds address chemistry, while CBT reshapes thinking.
Depression doesn’t exist in a vacuum; it’s part of a broader group called mood disorders, conditions where emotional states are unusually intense or prolonged. This group includes bipolar disorder, cyclothymia, and seasonal affective disorder. Knowing that depression falls under this umbrella helps clinicians choose the right treatment pathway and alerts patients that symptoms might overlap with other conditions.
Semantic triple: Depression encompasses mood disorders. Semantic triple: Effective treatment of depression often involves antidepressant medication. Semantic triple: Cognitive behavioral therapy influences depression recovery. These connections guide how we approach care, from diagnosis to daily coping strategies.
Beyond meds and therapy, lifestyle tweaks matter. Regular exercise releases endorphins, improves sleep quality, and reduces stress hormones. A balanced diet rich in omega‑3 fatty acids, B‑vitamins, and magnesium supports brain health. Even small habits—like a daily walk or a 10‑minute mindfulness session—can shift the brain’s chemistry over time, making other treatments more effective.
Social support is another pillar. Friends, family, or support groups provide accountability and reduce isolation, which fuels depressive thoughts. If you feel uncomfortable sharing with close ones, online communities or mental‑health hotlines can offer a safe space to vent and get advice.
It’s also critical to screen for medical issues that mimic or worsen depression. Thyroid problems, vitamin D deficiency, and chronic pain can all trigger low mood. A simple blood test or physical exam often uncovers these hidden factors, allowing doctors to treat the root cause alongside mental‑health interventions.
When you’re on antidepressants, monitoring side effects and progress is key. Common issues include weight changes, sleep disturbances, or temporary anxiety spikes. Keeping a mood journal helps you and your prescriber spot patterns, adjust dosages, or switch medications if needed. Remember, finding the right pill can take weeks, so patience and open communication are essential.
Finally, crisis planning should never be ignored. If thoughts of self‑harm arise, reach out immediately to a trusted person or emergency services. Having a written plan—who to call, where to go, and what steps to take—can save precious minutes and keep you safe.
Now that you’ve got a solid overview of depression, its related mood disorders, medication options, therapy techniques, and lifestyle factors, you’re ready to explore the detailed articles below. Each piece dives deeper into specific treatments, real‑world tips, and the latest research, giving you the tools to manage depression effectively.
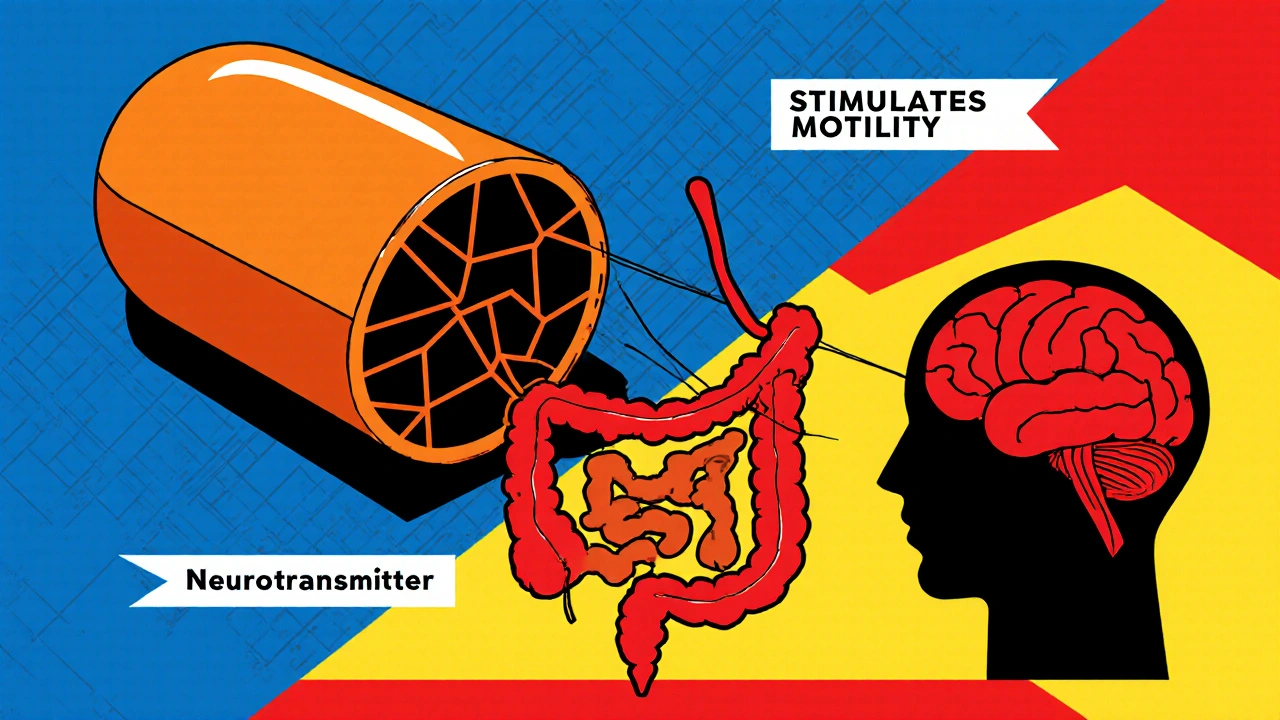
How Bisacodyl Affects Mental Health: Risks, Evidence, and Safe Use
Explore how Bisacodyl, a common stimulant laxative, can affect mental health. Learn the science, risks, and safe-use tips to protect your mood while relieving constipation.
Continue reading
How Spastic Muscle States Affect Mental Health
Explore how spastic muscle states like those in cerebral palsy, MS, or stroke raise depression and anxiety risks, and discover practical steps to improve both physical tone and mental well‑being.
Continue reading