SEARCH
Antiretroviral Therapy: What It Is, How It Works, and What You Need to Know
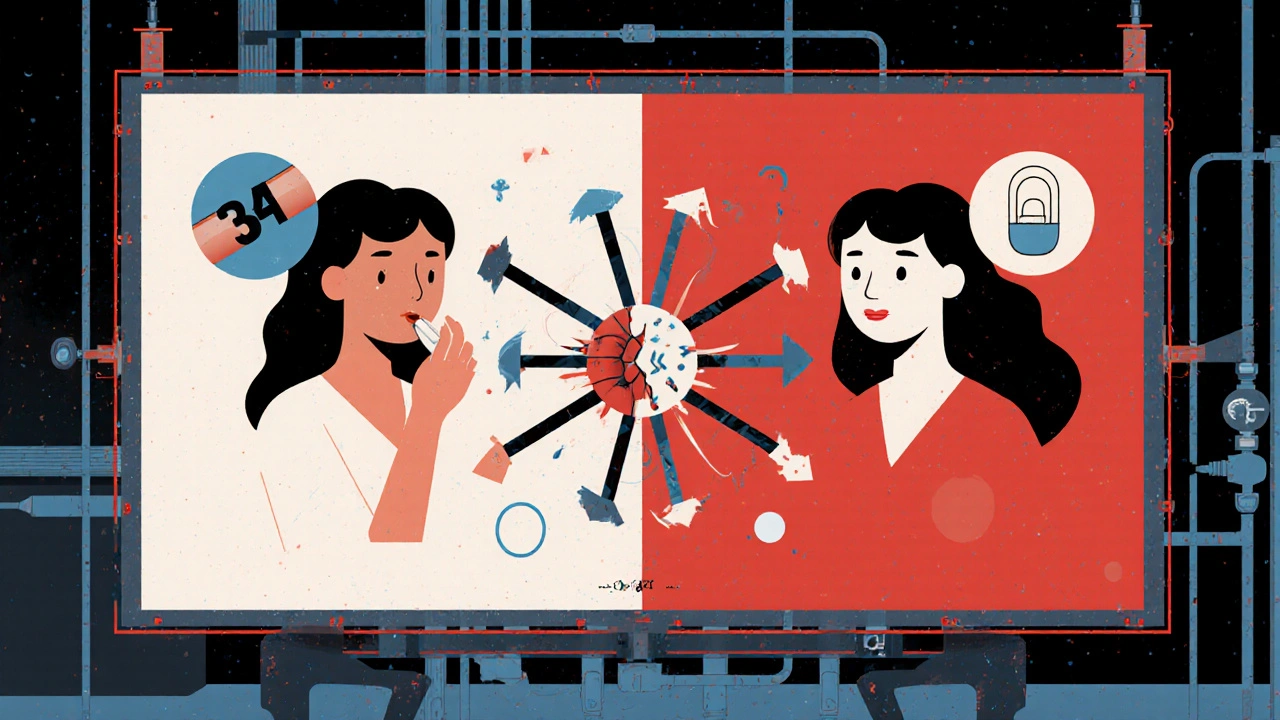
When someone is diagnosed with antiretroviral therapy, a combination of medications used to treat HIV by blocking the virus at different stages of its life cycle. Also known as ART, it doesn’t cure HIV—but it stops the virus from taking over the body, letting the immune system recover and stay strong. This isn’t just one drug. It’s usually three or more medicines from different classes, taken every day, designed to keep the virus so low it can’t be detected in blood tests. That’s called viral suppression, and it’s the goal of every treatment plan.
Antiretroviral therapy works because HIV is sneaky—it mutates fast. If you only take one drug, the virus adapts and fights back. But when you hit it with multiple drugs at once, it can’t escape. That’s why regimens include drugs like NRTIs, nucleoside reverse transcriptase inhibitors that block HIV from copying its genetic material, NNRTIs, non-nucleoside reverse transcriptase inhibitors that disable the enzyme HIV needs to replicate, and integrase inhibitors, drugs that stop HIV from inserting its DNA into human cells. These aren’t just labels—they’re the reason someone on treatment can live decades without progressing to AIDS.
Adherence is everything. Missing doses—even just one or two—can let the virus bounce back and become resistant. That’s why tools like medication logs, pill organizers, and phone reminders are so common in HIV care. It’s not about being perfect. It’s about being consistent. And when people stick with it, the results are powerful: not only do they stay healthy, but they can’t pass HIV to others. That’s prevention through treatment, and it’s changed the entire course of the epidemic.
Side effects used to be a big problem—nausea, fatigue, nerve pain. Today’s regimens are lighter. Many people take just one pill a day with few noticeable side effects. But some still struggle. That’s why doctors now match drugs to individual needs: kidney health, liver function, mental health, and even lifestyle. A person with diabetes might avoid certain drugs. Someone with depression might need one that doesn’t affect mood. This isn’t one-size-fits-all medicine. It’s personalized care.
There’s also the question of generics. Many antiretrovirals now come as affordable versions that work just as well as the brand names. You don’t need to pay more to get the same protection. And with advances in long-acting injectables, some people are moving away from daily pills altogether—getting shots every month or two. It’s a shift that’s making treatment easier for those who find daily routines hard to keep.
What you’ll find below are real stories and practical guides from people living with HIV. How to manage side effects like nausea. How to use a pill diary to stay on track. How to spot dangerous drug interactions. How to talk to your pharmacist about switching meds. These aren’t theoretical tips. They’re what works for real people on antiretroviral therapy, day after day.
HIV Protease Inhibitors and Birth Control: What You Need to Know About Reduced Contraceptive Effectiveness
HIV protease inhibitors can reduce the effectiveness of hormonal birth control, leading to unintended pregnancies. Learn which methods are risky, which are safe, and what to do if you're on antiretroviral therapy.
Continue reading