SEARCH
Lithium: What It Is, How It's Used, and What You Need to Know
When doctors talk about lithium, a naturally occurring salt used as a mood-stabilizing medication. Also known as lithium carbonate, it's one of the oldest and most studied treatments for bipolar disorder, a mental health condition marked by extreme mood shifts between highs and lows. Unlike newer drugs, lithium doesn’t just mask symptoms—it helps reset how the brain handles emotion and energy over time.
Lithium works by influencing chemicals in the brain like serotonin and dopamine, but it’s not fully understood why it helps some people so much. What we do know is that it reduces the frequency and severity of manic episodes and can also help prevent depressive crashes. It’s not a quick fix—it takes weeks to build up in your system and show results. That’s why doctors start low and go slow, watching your blood levels closely. Too little won’t help. Too much can be dangerous. That’s why regular blood tests are non-negotiable if you’re on lithium. Levels need to stay between 0.6 and 1.0 mmol/L for most people. Even small changes in diet, hydration, or other meds can throw that balance off.
It’s not just about the brain. Lithium affects your kidneys, thyroid, and even your weight. Many people gain a few pounds, feel more thirsty, or get mild tremors in their hands. Some develop an underactive thyroid, which is easy to fix with a daily pill. Kidney function can slowly decline over years, so annual checks are standard. These aren’t scary side effects—they’re manageable ones, if you’re monitored. That’s why lithium isn’t for everyone, but for those it helps, it’s life-changing. People who’ve tried six other meds and still struggled with cycling moods often say lithium is the one that finally brought them stability.
It’s also used off-label for things like depression that doesn’t respond to SSRIs, or to boost the effect of other antidepressants. But its biggest role is still in bipolar disorder, where it’s been the gold standard since the 1970s. Even with newer drugs like lamotrigine or valproate, lithium remains the only one proven to lower suicide risk in bipolar patients. That’s huge. Suicide is the leading cause of early death in people with this condition. Lithium doesn’t just calm mood swings—it saves lives.
There’s a myth that lithium is outdated. It’s not. It’s just old. And old doesn’t mean broken. It means tested. Thousands of studies, decades of real-world use, and millions of people who’ve stayed stable because of it. The challenge isn’t that lithium doesn’t work—it’s that it needs care. You need to take it every day, drink enough water, avoid too much salt, and get your blood checked. If you can do that, it’s one of the most reliable tools in psychiatry.
Below, you’ll find real stories and facts from people who’ve lived with lithium—what worked, what didn’t, and what they wish they’d known before starting. Whether you’re considering it, already on it, or just curious, these posts give you the unfiltered truth behind the prescription.
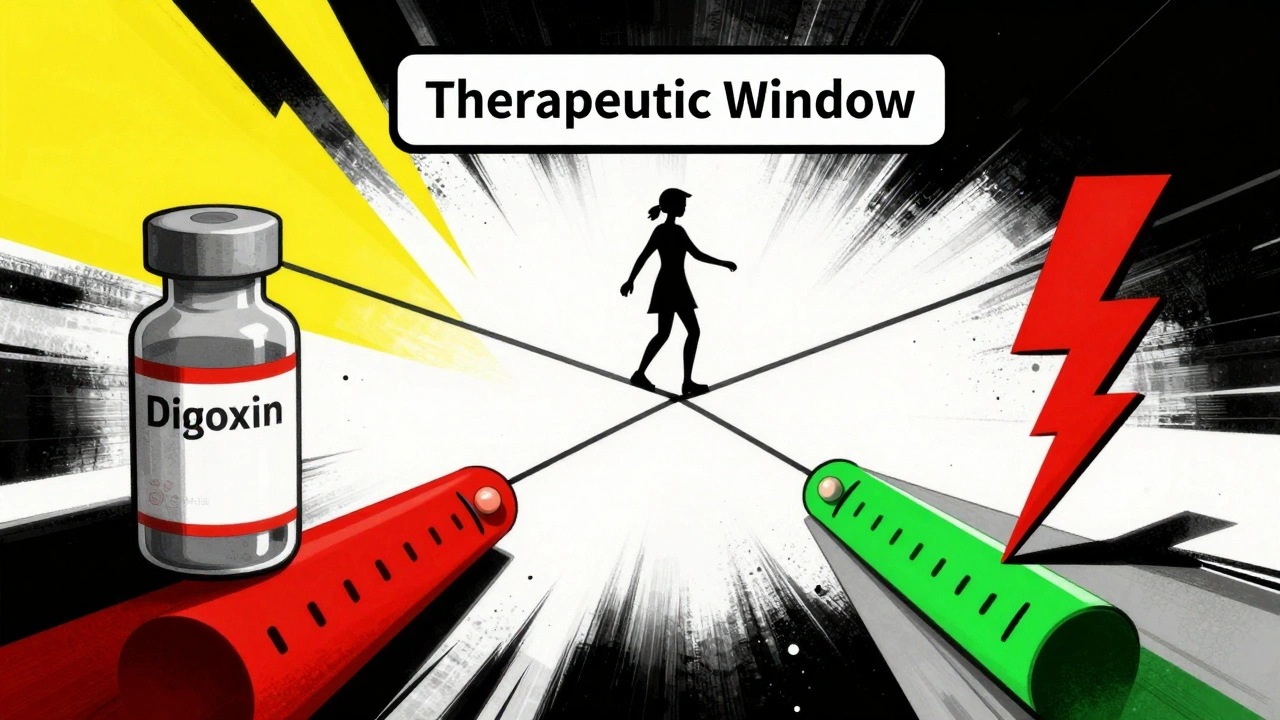
NTI Drug List: Common Medications with Narrow Therapeutic Windows
NTI drugs have a tiny margin between effective and toxic doses. Common examples include warfarin, lithium, digoxin, phenytoin, and tacrolimus. These require strict monitoring and careful dosing to avoid serious harm.
Continue reading