SEARCH
Warfarin: What It Is, How It Interacts with Antibiotics, and How to Stay Safe
When you take warfarin, an anticoagulant medication used to prevent dangerous blood clots. Also known as Coumadin, it works by blocking vitamin K, which your body needs to form clots. But this same mechanism makes warfarin tricky to manage — too little and you risk a stroke or clot, too much and you could bleed internally without warning. That’s why millions of people on warfarin need to be extra careful with what else they take — especially common antibiotics.
Many antibiotics, drugs used to treat bacterial infections can sharply raise your INR, the number doctors use to measure how long your blood takes to clot. A spike in INR means your blood is thinning faster than it should. Some antibiotics — like sulfamethoxazole/trimethoprim (Bactrim) and metronidazole — are especially risky. Even a short course can turn a stable dose into a medical emergency. That’s why checking your INR within a few days of starting an antibiotic isn’t optional — it’s life-saving.
And it’s not just antibiotics. INR monitoring, the regular blood test that tracks warfarin’s effect is your best defense. Skipping tests because you feel fine is a common mistake. Warfarin doesn’t cause symptoms when it’s too strong — until you start bleeding. Bruising easily, nosebleeds, dark stools, or sudden headaches could mean trouble. Your doctor might adjust your dose based on diet, alcohol, or even changes in your sleep or stress levels. There’s no one-size-fits-all dose. What worked last month might need tweaking this week.
Many people on warfarin also take other meds — statins for cholesterol, painkillers, or supplements like fish oil or vitamin K. Each one can shift how warfarin works. That’s why keeping a simple medication log, a daily record of every pill you take, including doses and times matters. It helps you and your doctor spot patterns before something goes wrong. A missed dose, a new antibiotic, even switching brands of warfarin — all of it adds up.
There’s no magic trick to warfarin. It’s not about being perfect. It’s about being aware. You don’t need to memorize every drug interaction. You just need to know: when you start a new medicine, ask if it affects warfarin. When you feel off, get your INR checked. When in doubt, don’t guess — call your pharmacist or doctor. The posts below give you real, practical stories from people who’ve been there — how antibiotics nearly caused a bleed, why one man switched to a different blood thinner, how a simple log kept a woman out of the ER. You’re not alone. And with the right info, you can take warfarin safely — for years, without fear.
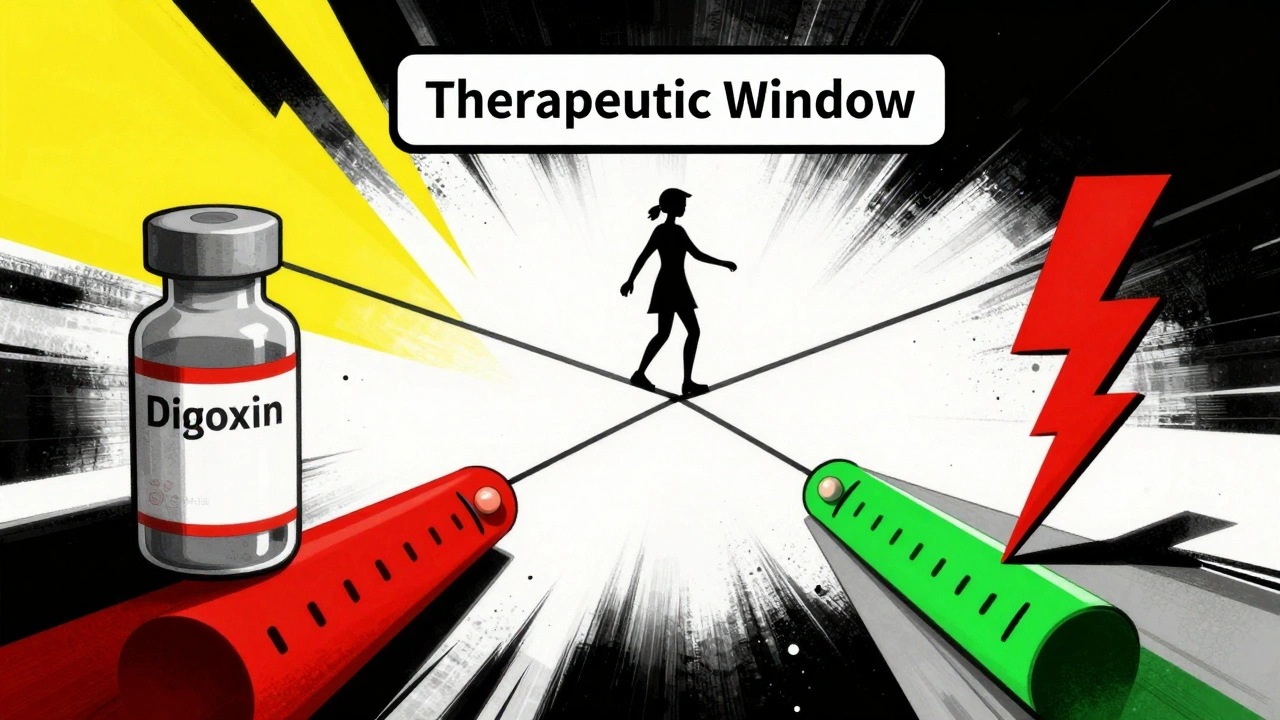
NTI Drug List: Common Medications with Narrow Therapeutic Windows
NTI drugs have a tiny margin between effective and toxic doses. Common examples include warfarin, lithium, digoxin, phenytoin, and tacrolimus. These require strict monitoring and careful dosing to avoid serious harm.
Continue reading