SEARCH
Warfarin Monitoring: What You Need to Know About Blood Tests and Safety
When you’re on warfarin, a blood thinner used to prevent dangerous clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. Also known as Coumadin, it’s one of the most common anticoagulants prescribed worldwide—but it doesn’t work unless you monitor it closely. Unlike newer blood thinners, warfarin doesn’t have a fixed dose. Your body processes it differently than anyone else’s, and even small changes in diet, other meds, or health can throw your levels off.
This is where INR testing, a simple blood test that measures how long it takes your blood to clot. Also known as International Normalized Ratio, it’s the only reliable way to know if your warfarin dose is too high, too low, or just right. A normal INR for someone on warfarin is usually between 2.0 and 3.0. Below that, you’re at risk for clots. Above it, you risk serious bleeding—like internal bleeding, nosebleeds that won’t stop, or brain hemorrhages. Your doctor will adjust your dose based on your INR, not guesswork.
Many things affect your INR. Eating a lot of leafy greens? That’s vitamin K, and it fights warfarin’s effect. Starting a new antibiotic? Some can make warfarin stronger. Drinking alcohol regularly? That can mess with your liver’s ability to process it. Even switching brands of warfarin can cause a shift. That’s why consistency matters: same meals, same time of day for your pill, same pharmacy. Skipping your INR test for a month? That’s how people end up in the ER.
Some people think once they’ve been on warfarin for years, they don’t need to test as often. That’s dangerous. Your body changes. Your kidneys slow down. Your diet shifts. You start a new supplement—like fish oil or garlic pills—that can thin your blood even more. One study from the American Heart Association found that nearly 40% of warfarin-related hospitalizations happened because patients skipped their INR checks.
There are tools to help. Home INR monitors let you prick your finger and get results in minutes, with data sent straight to your doctor. Not everyone qualifies, but if you’re stable and motivated, it cuts down on clinic visits. Still, you can’t skip the human check-in. Your pharmacist can spot drug interactions. Your nurse can notice signs of bruising or bleeding you might ignore.
And while newer blood thinners like apixaban or rivaroxaban don’t need routine testing, they’re not right for everyone. If you have mechanical heart valves, kidney problems, or a history of clots that didn’t respond to other drugs, warfarin is still the gold standard. But only if you treat it like the powerful, precise tool it is—not just another pill you swallow.
Below, you’ll find real stories and science-backed advice on managing warfarin safely: how to track your INR, what foods to watch, how to avoid dangerous interactions, and what to do when things go wrong. No fluff. Just what works.
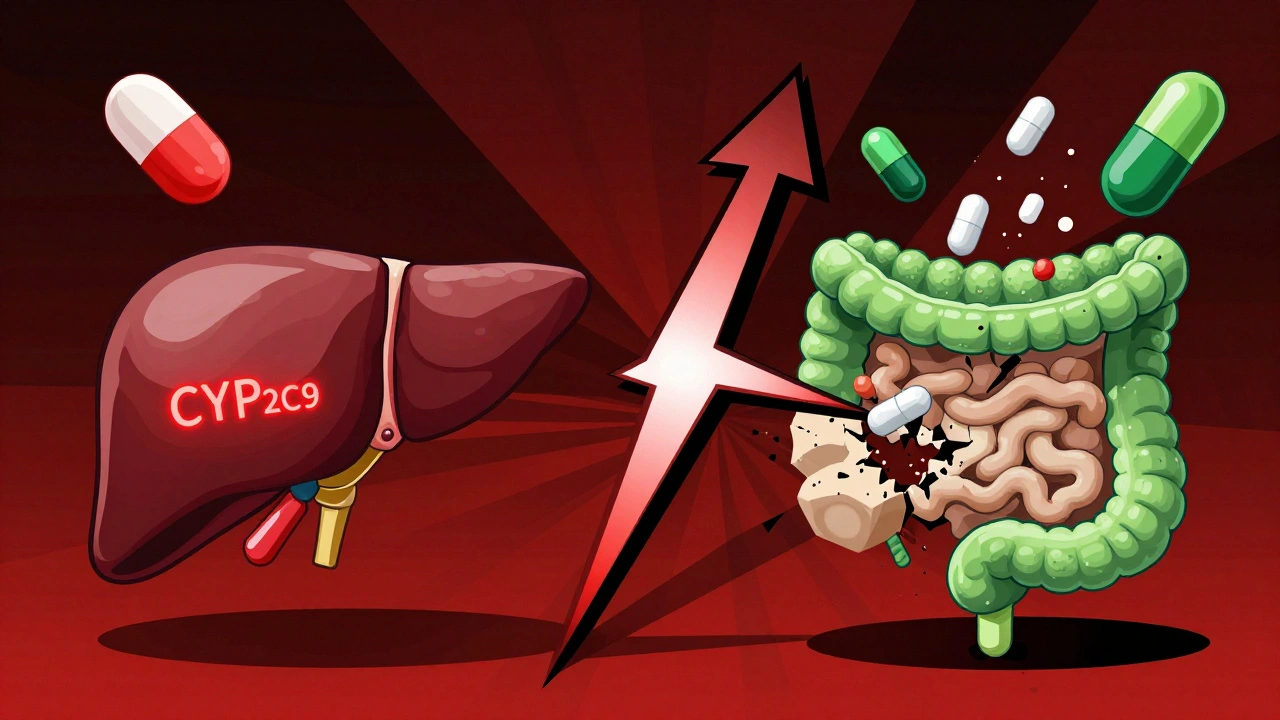
Antibiotics and Warfarin: How to Prevent Dangerous INR Spikes and Bleeding
Antibiotics can dangerously raise INR levels in people taking warfarin, increasing bleeding risk. Learn which antibiotics are most dangerous, when to check your INR, and how to prevent life-threatening spikes.
Continue reading