SEARCH
Brand Name Drugs: What They Are, Why They Cost More, and What You Need to Know
When you hear brand name drugs, the original versions of medications developed and marketed by pharmaceutical companies under a patent-protected name. Also known as originator drugs, they’re the first to hit the market after years of research and clinical trials. Think of them as the first version of a product—like the original iPhone before all the cheaper clones came out. They’re not necessarily better, but they come with a price tag that reflects the cost of development, marketing, and exclusivity.
That’s where generic medications, chemically identical versions of brand name drugs sold after the patent expires. Also known as generic drugs, they work the same way, have the same side effects, and are approved by the same agencies—but often cost 80% less. Many people worry generics aren’t as strong or safe, but the science says otherwise. The FDA requires them to match brand name drugs in active ingredients, strength, and how they’re absorbed. The difference? The fillers, color, and packaging. Your body doesn’t care about the logo on the bottle.
Why do some doctors still push brand name drugs? Sometimes it’s habit. Sometimes it’s pressure from reps. But more often, patients don’t know they can ask for the cheaper version. And when they do, pharmacists can usually switch it unless the prescription says "do not substitute." That little note? It’s not always medical—it’s often financial. Insurance companies sometimes prefer generics, but not always. And if you’re paying out of pocket, the gap can be huge. A brand name drug might cost $300 a month. The generic? $15.
Drug pricing, the cost of medications set by manufacturers, insurers, and pharmacies, often with little transparency. Also known as pharmaceutical costs, it’s one of the biggest frustrations in healthcare today. Why does a pill that costs pennies to make sell for hundreds? It’s not just R&D. It’s patents, marketing, and loopholes that let companies extend exclusivity by tweaking formulas slightly. Some brand name drugs have been on the market for decades but still charge premium prices because no generic has been approved yet—often due to legal delays, not science.
Then there’s medication safety, the practice of using drugs correctly to avoid harm, overdose, or dangerous interactions. Also known as drug safety, it applies whether you’re on a brand name or generic. Mixing pills without tracking them? That’s how overdoses happen. Not because the drug is bad—but because you didn’t know what else you were taking. That’s why so many posts here talk about medication logs, interaction checkers, and simplifying regimens. The brand name doesn’t make you safer. Your awareness does.
You’ll find posts here that cut through the noise: why people distrust generics even when they work just as well, how to spot fake pills that look like brand name drugs, and how to save money without risking your health. You’ll see how drugs like Ozempic or Zoloft have generics now—and why switching might be smarter than sticking with the name you recognize. You’ll learn when a brand name actually matters—like with thyroid meds or blood thinners—where tiny differences in absorption can make a real impact.
Brand name drugs aren’t the enemy. But they’re not always the answer. Knowing the difference between marketing and medicine? That’s the real power move. And it’s not about being loyal to a label. It’s about being smart with your health—and your wallet.
What Are Authorized Generics? Complete Explanation
Authorized generics are identical to brand-name drugs in every way-same ingredients, same manufacturer, same factory-just without the brand label. Learn how they work, why they exist, and how they can save you money without compromising quality.
Continue reading
Authorized Generics: Same Drug, Different Label - What You Need to Know
Authorized generics are identical to brand-name drugs but sold under a generic label. Learn how they work, why they’re cheaper, and how to spot them - without sacrificing quality or safety.
Continue reading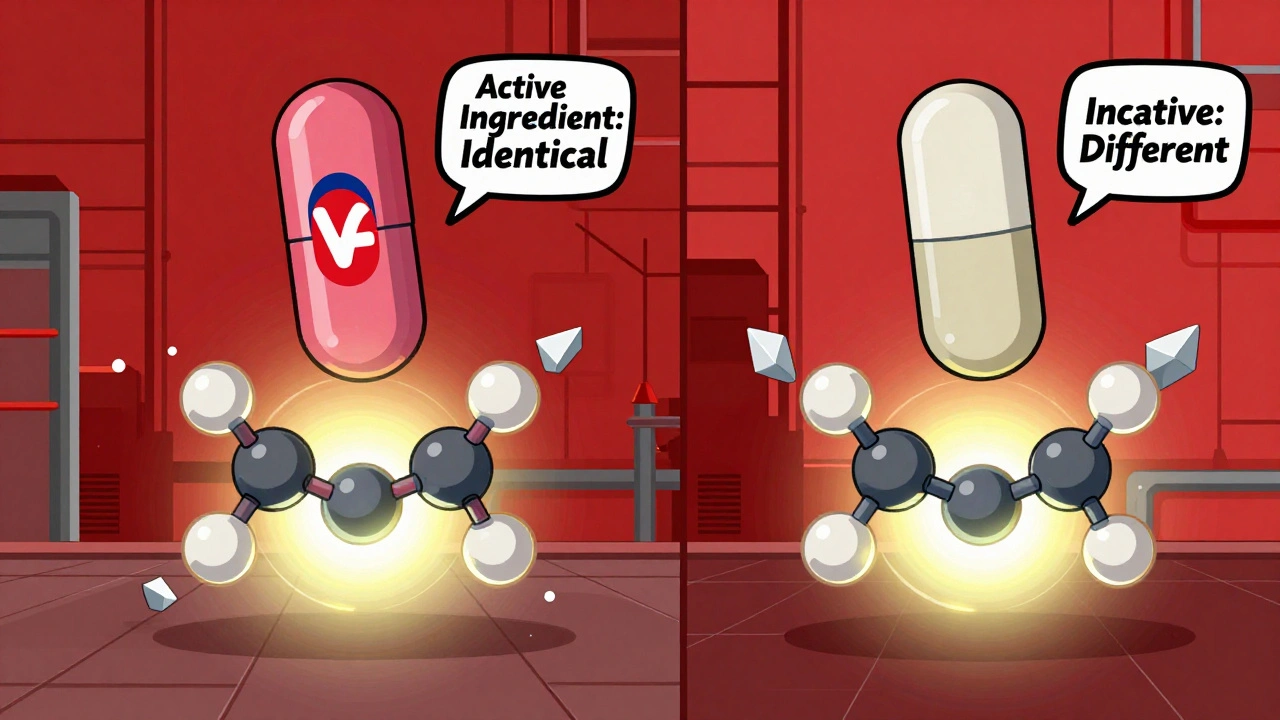
Are Generic Drugs Copies? The Truth Behind the Myth
Generic drugs are not copies - they're FDA-approved equivalents with the same active ingredients as brand-name medications. Learn the science behind why they work the same, cost 85% less, and are safe for most people.
Continue reading
Authorized Generic Pricing: Why They Cost Less Than Brand-Name Drugs
Authorized generics are identical to brand-name drugs but cost less because they skip marketing and branding expenses. Learn how they work, why they're cheaper, and how to get them to save on prescriptions.
Continue reading
Therapeutic Equivalence: Are Authorized Generics Really the Same as Brand Drugs?
Authorized generics are the exact same medication as brand-name drugs-same ingredients, same manufacturer, same quality. Learn why they’re a safe, cost-effective alternative and how to identify them.
Continue reading